Amiodarone, Digoxin, and Warfarin: The Dangerous Drug Triad You Can't Ignore
29 Oct, 2025Drug Interaction Management Calculator
Input Current Medication Doses
Enter your current doses to calculate safe adjustments when starting amiodarone
Recommended Adjustments
Calculations will appear here after you click the button
Important Safety Notes
The FDA recommends:
- Reduce digoxin by 50% immediately when starting amiodarone
- Reduce warfarin by 30-50% when starting amiodarone
- Check INR every 48-72 hours for first 2 weeks
- Check digoxin levels 72 hours after starting amiodarone
Signs to Watch For
If you experience any of these, contact your doctor immediately:
- Nausea, vomiting, blurred/yellow vision
- Confusion or dizziness
- Irregular heartbeat
- Unusual bruising or bleeding
- Severe headache or dizziness
Imagine taking three common heart medications - amiodarone, digoxin, and warfarin - because your doctor says they’re necessary. You’re not alone. Thousands of people with atrial fibrillation are on this exact combo. But here’s the problem: together, they can turn deadly. This isn’t a rare edge case. It’s a well-documented, preventable medical trap that kills people every year - and most don’t see it coming.
Why This Trio Is So Dangerous
Amiodarone is a powerful antiarrhythmic used to treat irregular heartbeats like atrial fibrillation and ventricular tachycardia. Digoxin helps slow the heart rate in those same conditions. Warfarin prevents clots, especially in people with AFib who are at risk of stroke. On their own, each drug is manageable. Together? They amplify each other’s effects in ways that are hard to predict - and even harder to reverse. The real danger lies in how amiodarone messes with how your body handles the other two. It doesn’t just interact with digoxin and warfarin - it traps them in your system. For digoxin, amiodarone blocks a key transporter called P-glycoprotein. This transporter normally pushes digoxin out of your cells and kidneys so it can be cleared. When it’s blocked, digoxin builds up. Studies show serum levels can jump 40% to 100% within just a few days of starting amiodarone. That’s not a small change. Digoxin toxicity kicks in at levels above 1.2 ng/mL - and in older adults, even 0.8 ng/mL can cause problems. Symptoms? Nausea, vomiting, blurry yellow vision, confusion, and dangerous heart rhythms like ventricular tachycardia. One 2021 study found that patients on both amiodarone and digoxin had a 23% higher risk of death than those on digoxin alone. With warfarin, the story is even more serious. Amiodarone and its metabolite, desethylamiodarone, shut down the liver enzymes (CYP2C9 and CYP3A4) that break down warfarin. This means warfarin sticks around longer, making your blood thinner than intended. The result? INR levels - the measure of how long your blood takes to clot - can skyrocket from a safe 2.5 to over 8 or 10 in just a week. An INR above 4.0 is dangerous. Above 6.0? You’re at high risk of internal bleeding. A 2020 study of over 12,000 patients showed amiodarone increased the risk of INR over 4.0 by more than 300%. And when digoxin levels rise too, they can displace warfarin from proteins in your blood, adding even more free warfarin into circulation. That’s a triple whammy.What Happens When Things Go Wrong
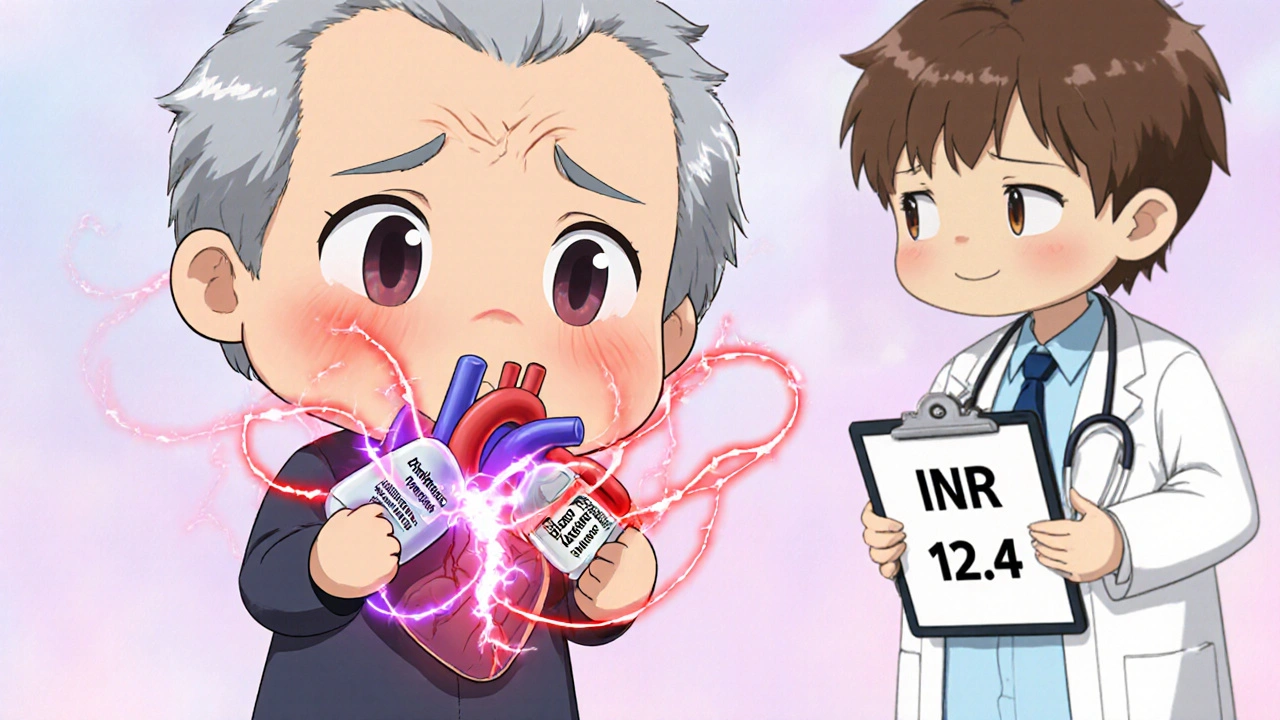
Real patients aren’t statistics. They’re people. A 78-year-old man in Brisbane was on warfarin for AFib after a previous stroke. His heart rate stayed high, so his cardiologist added digoxin. Then, he developed frequent palpitations - amiodarone was added. Within 10 days, he started vomiting, felt dizzy, and fell. His INR was 12.4. He needed four units of fresh frozen plasma and a high dose of vitamin K. He survived, but spent three weeks in hospital. The FDA’s adverse event database recorded 1,842 cases of digoxin toxicity linked to amiodarone between 2010 and 2022. That’s more than five times the rate seen without amiodarone. For warfarin, the numbers are worse: 387 deaths in 2022 alone were tied to this triad. And those are just the reported cases. Many more go unreported. The worst part? These events often happen in the first 30 days - when doctors and patients think everything’s fine. People assume if they’ve been on the same meds for months, adding one more won’t hurt. But amiodarone doesn’t work like other drugs. It lingers. Its half-life is 25 to 100 days. That means even after you stop taking it, the interaction keeps going for weeks. You can’t just stop and restart like flipping a switch.How to Manage This Triad - If You Must Use It
The truth? Many patients don’t need all three. Direct oral anticoagulants (DOACs) like apixaban or rivaroxaban have replaced warfarin in 82% of new AFib cases since 2022. If you’re new to treatment, ask: do I really need warfarin? But if you’re already on this combo - and many older patients are, especially with mechanical heart valves - you need a strict plan:- Reduce digoxin by 50% immediately when amiodarone starts. Don’t wait for symptoms. Don’t wait for a blood test. Start low.
- Check serum digoxin levels 72 hours after starting amiodarone. Repeat weekly until stable. Target level: below 0.8 ng/mL in elderly patients.
- Reduce warfarin by 30-50% before or at the same time as starting amiodarone. Many doctors miss this step and wait too long.
- Check INR every 48 to 72 hours for the first two weeks, then weekly for at least four weeks. Don’t rely on one number - look at the trend. A sudden jump from 2.6 to 3.8 in three days? That’s a red flag.
- Keep monitoring for 4 to 6 weeks after stopping amiodarone. The drug doesn’t leave your body quickly. Your warfarin dose may need to be increased again slowly.
What Your Doctor Should Be Doing
This isn’t just about you. It’s about systems. A 2022 study in JAMA Internal Medicine found that hospitals using electronic health records with built-in alerts for this interaction reduced medication errors by 65%. If your doctor’s system doesn’t flag this combo, ask why. The American College of Cardiology’s 2022 update says this interaction is one of the most preventable causes of iatrogenic harm in cardiology. That’s a fancy way of saying: it’s not a mistake - it’s negligence if it’s not managed properly. Your doctor should be:- Documenting why all three drugs are still needed
- Checking for alternatives - like switching from warfarin to a DOAC
- Using a medication reconciliation tool every time a new drug is added
- Discussing signs of digoxin toxicity and bleeding risks with you - not just handing you a prescription
Genetics and Other Risk Factors
Not everyone reacts the same way. A 2023 study in Clinical Pharmacology & Therapeutics found that people with a specific genetic variant (ABCB1 C3435T TT genotype) had up to 92% higher digoxin levels when on amiodarone - compared to 58% in those without the variant. If you’re of European descent, you’re more likely to have this variant. Age matters too. Over 63% of reported cases involve patients over 75. Kidney function declines with age, and digoxin is cleared through the kidneys. Warfarin metabolism slows too. The body’s ability to handle these drugs drops - but doses often don’t. Even diet can play a role. Vitamin K intake (from leafy greens) affects warfarin. If you suddenly eat more kale or spinach, your INR can drop. But if you’re on amiodarone, your warfarin is already unstable - so even small changes can cause big swings.What You Can Do Today
If you’re on amiodarone, digoxin, and warfarin:- Ask your pharmacist to run a full drug interaction check - don’t assume your doctor did.
- Keep a log of your INR values and digoxin levels. Bring it to every appointment.
- Know the signs of digoxin toxicity: nausea, vomiting, blurred vision (especially yellow or green halos), irregular heartbeat, confusion.
- Know the signs of bleeding: unusual bruising, nosebleeds that won’t stop, blood in urine or stool, severe headaches, dizziness.
- If you fall or hit your head - get checked immediately. Even a minor bump can cause internal bleeding if your INR is high.
- Ask: Is there a safer alternative? Could I switch to a DOAC? Could I stop digoxin if my heart rate is controlled another way?
The Bigger Picture
This triad isn’t going away. The American Heart Association estimates 4.3 million Americans will still need this combination by 2030 - mostly because they have mechanical heart valves, can’t afford DOACs, or have been on warfarin for decades. But that doesn’t mean it’s acceptable. The FDA added a Black Box Warning to amiodarone in 2023 - the strongest possible alert - citing over 2,100 serious events and 387 deaths in 2022 alone. That number is rising. We’re not talking about rare side effects. We’re talking about predictable, preventable harm. This interaction is not a mystery. It’s been studied since the 1980s. We know exactly how to manage it. We just don’t always do it. If you’re on this combo, you’re not just taking medication - you’re managing a ticking clock. The good news? You can stop it - if you know what to look for, and if you ask the right questions.Can I take amiodarone with digoxin and warfarin safely?
Yes - but only under strict medical supervision. Amiodarone significantly increases levels of both digoxin and warfarin, raising the risk of toxicity and bleeding. It’s not impossible, but it’s high-risk. Doses must be reduced upfront, levels must be monitored frequently, and alternatives should be considered. Never start or stop any of these drugs without your doctor’s guidance.
How long does the interaction last after stopping amiodarone?
Amiodarone has an extremely long half-life - between 25 and 100 days. That means its effects on digoxin and warfarin can last for weeks to months after you stop taking it. INR and digoxin levels must be monitored for at least 4 to 6 weeks after discontinuation. Many patients need to gradually increase their warfarin dose again during this time.
Should I switch from warfarin to a DOAC if I’m on amiodarone?
It depends. Amiodarone still inhibits P-glycoprotein, which affects DOACs like dabigatran - so the interaction isn’t gone. But DOACs don’t require INR monitoring and have a lower risk of major bleeding than warfarin. For most people, switching from warfarin to a DOAC reduces overall risk. Talk to your cardiologist about whether you’re a candidate - especially if you don’t have a mechanical heart valve.
What are the early signs of digoxin toxicity?
Early signs include nausea, vomiting, loss of appetite, fatigue, and dizziness. Visual changes - like seeing yellow or green halos around lights - are classic but not always present. Heart rhythm changes, such as a slow or irregular pulse, are serious red flags. If you notice any of these, contact your doctor immediately. Don’t wait for a blood test.
Is this interaction more dangerous for older adults?
Yes. Older adults are at higher risk because their kidneys clear digoxin more slowly, their liver processes warfarin less efficiently, and they’re more likely to have other health conditions that increase bleeding risk. Studies show over 60% of serious cases involve patients over 75. Dose reductions should be more aggressive in this group - and monitoring should be more frequent.
Can I take supplements or herbal products with this combination?
Avoid most supplements. St. John’s Wort can reduce warfarin’s effect. Garlic, ginkgo, and ginger can increase bleeding risk. Even vitamin K supplements can interfere with warfarin if taken inconsistently. Always tell your doctor or pharmacist about everything you’re taking - including vitamins, herbs, and over-the-counter meds. Many interactions aren’t listed on drug labels.
Jackson Olsen
October 30, 2025 AT 20:33This is wild I had no idea amiodarone could mess with warfarin like that
Amanda Nicolson
October 31, 2025 AT 13:26I’m a nurse and I’ve seen this happen way too often. A sweet 82-year-old lady came in last month with an INR of 11 after her cardiologist added amiodarone. She didn’t even know she was on digoxin - her family doctor prescribed it years ago and no one ever reviewed it. She had a brain bleed. Survived, but now she can’t walk. This isn’t just a drug interaction - it’s a systemic failure. Doctors are overworked, patients are confused, and no one’s checking the damn interactions before writing scripts. We need mandatory EHR alerts. Like, now.
Emily Kidd
November 1, 2025 AT 01:23my grandma was on this combo and her doc never told her about the yellow vision thing. she thought it was just old age. then she fell and broke her hip. turned out her digoxin was sky high. they had to give her vitamin k and fluids for days. don’t assume your doctor knows everything. ask for the levels. keep a log. seriously.
Niki Tiki
November 2, 2025 AT 09:37why are we still using warfarin in 2024? it’s 1950s medicine. DOACs are cheaper now and don’t require weekly blood tests. if your doc still pushes warfarin they’re either lazy or getting kickbacks from pharma. stop letting them play Russian roulette with your life
MOLLY SURNO
November 4, 2025 AT 07:03This is an exceptionally well-researched and sobering post. The data on digoxin toxicity and INR spikes is alarming, and the clinical recommendations are clear and actionable. I’ve shared this with my cardiology team. We’re implementing a checklist for patients on amiodarone - including mandatory baseline and follow-up levels for both digoxin and INR. Prevention is not optional. Thank you for writing this.
Alex Hundert
November 6, 2025 AT 02:14Listen. If you’re on this combo and your doctor hasn’t reduced your digoxin by 50% before starting amiodarone - fire them. No exceptions. I’ve been in this field 18 years and I still see this mistake. It’s not ignorance - it’s negligence. And it kills. You deserve better. Demand a pharmacist consult. Demand a review. Your life isn’t a trial run.
Arrieta Larsen
November 6, 2025 AT 10:23I’ve been on all three for 7 years. My INR’s been stable because I track everything. I take my digoxin at 8am, check my INR every 10 days, and avoid kale like it’s poison. It’s a lot of work. But I’m alive. So if you’re on this combo - be the patient who asks. Be the one who writes it down. You’re not being annoying. You’re saving your own life.
Penny Clark
November 6, 2025 AT 20:49my uncle died from this… i didn’t even know it was possible for meds to do that. he was just trying to live. he had afib and a stroke before. they kept adding pills like they were fixing a leaky faucet. but it was a bomb. i wish i’d known. now i’m telling everyone. please share this. someone might live because you did.
Justin Cheah
November 7, 2025 AT 21:32think about it. amiodarone was approved in the 80s. the interaction with warfarin was known by 1992. the FDA knew. the AMA knew. but they kept pushing it because it’s profitable. Big Pharma doesn’t care if you bleed out as long as you’re on their drugs. DOACs cost more? good. that means more profit. they don’t want you switching. they want you dependent. this isn’t medicine - it’s a money trap. and your doctor? they’re probably on their payroll. ask for the financial disclosures. you have the right.
Scott Dill
November 8, 2025 AT 19:25yo if you’re on this combo and you’re not checking your levels - stop reading and go call your pharmacy right now. like, right now. i’m not joking. i’ve seen people get dizzy and think it’s just stress. then they’re in the ER with a brain bleed. you’re not invincible. your meds aren’t harmless. take 5 minutes. call. ask. save yourself.
Mike Gordon
November 9, 2025 AT 22:08my dad was on this combo for 10 years. we didn’t know any of this until his INR hit 9. he was lucky. he survived. but now he’s on rivaroxaban and off digoxin. his energy’s back. he’s hiking again. i wish we’d known sooner. please, if you’re reading this - ask your doc about alternatives. don’t wait for a crisis. the best treatment is the one you don’t need.
Kathy Pilkinton
November 11, 2025 AT 11:06oh wow so the ‘standard of care’ is literally a death sentence? congrats, medicine. you’ve turned a simple heart condition into a full-time job for patients. and if you’re over 70? you’re just a walking lab experiment. nice. i’m sure the board members are sleeping well. maybe next they’ll add lithium and methotrexate to the mix. why not? more blood tests, more bills, more ‘oops we didn’t warn you’ moments.
Holly Dorger
November 11, 2025 AT 12:22my mom is 81 and on all three. she’s terrified now after reading this. i printed it out and took it to her cardiologist. he said ‘we monitor her closely’ - but didn’t know the 50% digoxin reduction rule. i had to show him the study. he changed her dose that day. thank you for this. i’m sharing it with every older person i know.
caiden gilbert
November 12, 2025 AT 19:28amiodarone is basically the ghost in the machine. it shows up, hangs around for months after you quit it, and messes with your meds like a spiteful roommate. you think you’re clean? nah. your liver’s still whispering to your kidneys about digoxin. and your warfarin? it’s still drunk. this ain’t a drug - it’s a lingering curse. treat it like one.
phenter mine
November 13, 2025 AT 13:16thanks for this post i had no idea about the genetic thing. i have the c3435t tt variant and my doc never tested for it. i’m gonna ask for a genetic panel next visit. if this saved one life it’s worth it