Bleeding Risk from SSRIs: How Platelet Dysfunction Increases Bleeding Danger
18 Feb, 2026When you take an SSRI to treat depression or anxiety, you’re not just changing your mood-you’re also affecting how your blood clots. It sounds surprising, but SSRIs can increase your risk of bleeding, even from small cuts or bruises. This isn’t a rare side effect. It’s a well-documented biological effect tied directly to how these drugs work inside your body. If you’re on an SSRI and notice you’re bruising more easily, bleeding longer after a nosebleed, or seeing dark stools after a meal, you’re not imagining it. There’s science behind it-and understanding how SSRIs interfere with platelets can help you make smarter choices about your treatment.
How SSRIs Work (And Why That Causes Bleeding)
SSRIs-Selective Serotonin Reuptake Inhibitors-were designed to boost serotonin in the brain. That’s how they help with depression: by keeping more serotonin available between nerve cells. But here’s the catch: serotonin isn’t just in your brain. About 99% of the serotonin in your entire body is stored in your platelets. These tiny blood cells use serotonin like a signal flare. When you cut yourself, platelets rush to the site, release their serotonin, and that serotonin tells other platelets to stick together and form a clot. It’s a critical part of stopping bleeding.
SSRIs block the serotonin transporter (5-HTT), the same protein that brings serotonin back into brain cells. But that same transporter is also on platelets. When an SSRI blocks it, platelets can’t refill their serotonin stores. Over time, they run low. Think of it like a flashlight with a dead battery. The platelets still show up when there’s damage, but they don’t have the signal to rally others. That’s why platelet aggregation-the clumping that forms clots-gets weaker. Studies show serotonin levels in platelets drop by over 80% in people taking paroxetine. That’s not a minor effect. That’s a major disruption in your body’s natural clotting system.
Not All SSRIs Are the Same
If you’ve been told all SSRIs are interchangeable, that’s misleading. Their ability to block the serotonin transporter varies significantly. This difference directly affects bleeding risk.
Paroxetine and fluvoxamine bind tightly to the transporter-with Ki values of 0.17 and 0.34 nanomolar, respectively. That means they’re very effective at blocking serotonin uptake. The result? Higher bleeding risk. Studies show paroxetine users have a 40-50% greater chance of upper GI bleeding compared to those on other antidepressants. Fluvoxamine isn’t far behind.
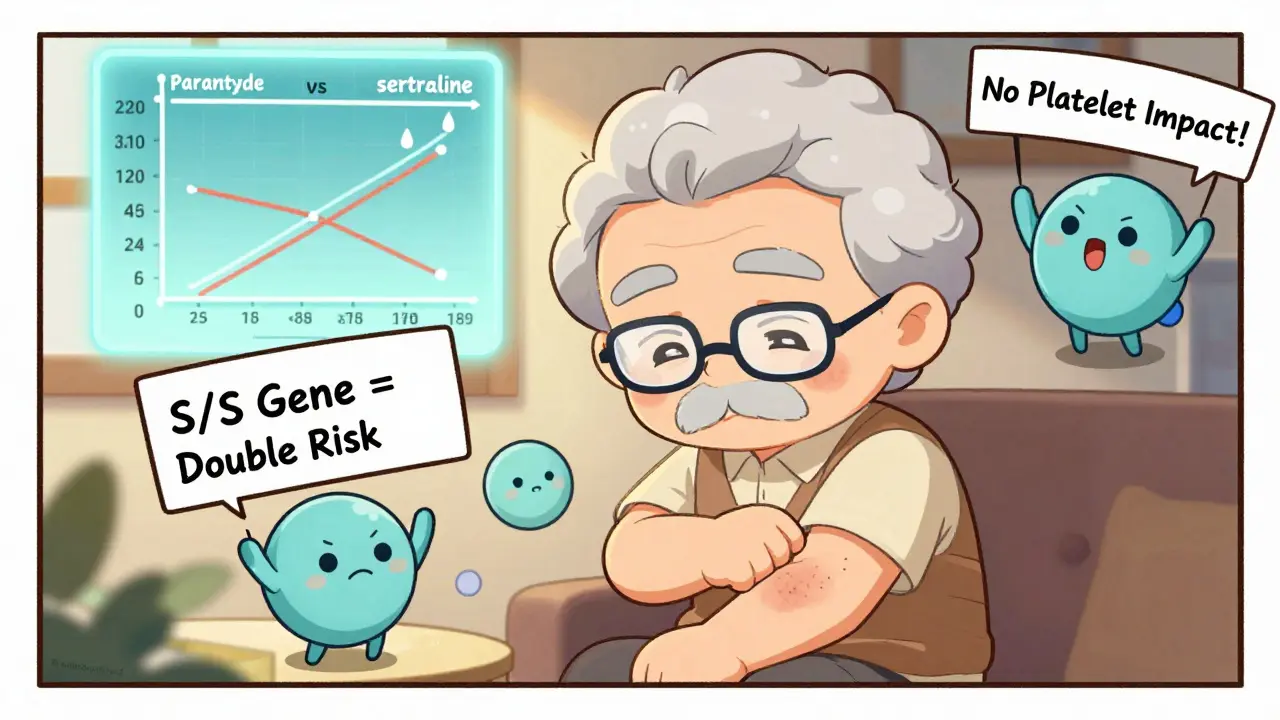
On the other end, sertraline and citalopram have lower binding affinity (Ki values of 0.52 and 0.91). Their effect on platelets is weaker. That’s why sertraline is often the go-to SSRI for patients with a history of bleeding or those on blood thinners. Data from the FDA’s adverse event database shows only 9.2% of sertraline users report easy bruising, compared to 18.7% of paroxetine users. It’s not just theory-it’s seen in real-world patient reports.
When Bleeding Risk Gets Dangerous
SSRIs alone can increase bleeding, but the real danger comes when they’re combined with other medications. The most common and dangerous combo is SSRIs with blood thinners like warfarin, apixaban, or rivaroxaban. A 2024 meta-analysis in JAMA Network Open found that people on both an SSRI and an oral anticoagulant had a 35% higher risk of major bleeding than those on anticoagulants alone. That’s not small. That’s a clear, measurable spike in risk.
NSAIDs-like ibuprofen, naproxen, or even aspirin-make things worse. A 2013 study found that combining SSRIs with NSAIDs increases bleeding risk by 4.5 times. Why? NSAIDs damage the stomach lining and inhibit another clotting pathway. Add low platelet serotonin on top of that, and your body has almost no way to stop bleeding.
Even surgery becomes riskier. A 2023 poll of doctors on Sermo found that 63% had seen increased bleeding during minor procedures like dental work or skin biopsies in SSRI users. While some patients can stay on their SSRI during cardiac surgery (because stopping it risks depression relapse), for other procedures, doctors often recommend stopping the SSRI 5-7 days beforehand. That’s not a guess-it’s based on how long it takes platelets to regenerate and refill their serotonin stores.
Who’s Most at Risk?
You can’t avoid all risk, but you can reduce it. The HAS-BLED score is a simple tool doctors use to assess bleeding risk. It looks at factors like high blood pressure, kidney or liver problems, past bleeding, age over 65, and whether you’re on other drugs that affect clotting. If your score is 3 or higher, you’re in the high-risk group. For those patients, switching from paroxetine to sertraline or citalopram can cut bleeding risk in half.
Another factor is genetics. A 2024 study in the Pharmacogenomics Journal found that people with two copies of the short version of the 5-HTTLPR gene (S/S genotype) had more than twice the bleeding risk on SSRIs compared to those with the long version (L/L). This isn’t routine testing yet-but it’s coming. By late 2025, the European Medicines Agency may require genetic risk labels on SSRI packaging.
Older adults are especially vulnerable. Their platelets don’t regenerate as quickly, and they’re more likely to be on multiple medications. A 2022 IQVIA analysis showed that paroxetine prescriptions dropped by 37% among older patients with stomach issues, while sertraline prescriptions rose by 28% in the same group. Doctors are already adjusting based on evidence.
What to Do If You’re on an SSRI
Don’t stop your medication without talking to your doctor. Depression itself carries serious risks-including higher chances of heart attacks and suicide. The goal isn’t to avoid SSRIs. It’s to use them safely.
- Check which SSRI you’re on. If it’s paroxetine or fluvoxamine, ask if switching to sertraline or citalopram is an option.
- Avoid NSAIDs. Use acetaminophen (Tylenol) for pain instead of ibuprofen or naproxen.
- Watch for warning signs. Unusual bruising, nosebleeds that last longer than usual, dark or tarry stools, or vomiting material that looks like coffee grounds? Get checked immediately.
- Tell every doctor you see. Dentists, surgeons, even your physical therapist need to know you’re on an SSRI. Many now have alerts in their systems, but it’s still your job to speak up.
- Consider alternatives. For high-risk patients, bupropion (Wellbutrin) or mirtazapine (Remeron) don’t affect platelets at all. They’re not SSRIs, but they work for depression too.
Real Stories, Real Risks
On Reddit’s r/SSRI community, a 2022 thread titled “SSRIs and unexpected bleeding” had over 300 comments. One man described how he started taking paroxetine for anxiety and within weeks, he was bruising from his shirt collar. Another woman said she had a nosebleed that lasted 45 minutes after a minor cold. Both switched to sertraline-and the bleeding stopped.
Drugs.com reviews from nearly 3,000 users showed that 12.4% reported easy bruising. Paroxetine users were twice as likely to report it as sertraline users. These aren’t outliers. They’re patterns.
Even in hospitals, the evidence is clear. Epic Systems, a major electronic health record company, found that when their system started warning doctors about SSRI-anticoagulant combos, prescriptions dropped by over 22%. That’s thousands of patients who avoided dangerous interactions just because they were alerted.
The Bottom Line
SSRIs save lives. But they also change how your blood behaves. Platelet dysfunction isn’t a side effect you can ignore. It’s a real, measurable, and preventable risk. The key is not to avoid SSRIs altogether, but to match the right one to your personal risk profile. If you’re young and healthy with no other medications, the risk is low. If you’re over 65, on blood thinners, or have a history of ulcers or bleeding, the choice matters more.
Ask your doctor: "Is this the safest SSRI for my situation?" and "Should I avoid NSAIDs or other drugs that increase bleeding?" The answer might mean switching from paroxetine to sertraline. Or it might mean avoiding ibuprofen for headaches. Small changes. Big impact.
Do all SSRIs cause bleeding?
No. Not all SSRIs carry the same bleeding risk. Paroxetine and fluvoxamine have the strongest effect on platelets because they bind tightly to the serotonin transporter. Sertraline and citalopram have weaker binding and lower bleeding risk. Switching from paroxetine to sertraline can reduce your bleeding risk by nearly half.
Can I take ibuprofen with an SSRI?
It’s not recommended. Combining SSRIs with NSAIDs like ibuprofen or naproxen increases bleeding risk by 4.5 times. Use acetaminophen (Tylenol) for pain relief instead. If you must take an NSAID, talk to your doctor about short-term use and monitor for signs of bleeding.
Should I stop my SSRI before surgery?
It depends. For major surgeries with high bleeding risk-like brain or spinal procedures-doctors often recommend stopping the SSRI 5 to 7 days beforehand. For cardiac surgery, guidelines suggest continuing because stopping can trigger depression relapse, which is dangerous. Always discuss this with your surgeon and psychiatrist together.
What are the signs of serious bleeding from SSRIs?
Watch for: black or tarry stools, vomiting blood or material that looks like coffee grounds, unexplained bruising that spreads quickly, nosebleeds lasting longer than 20 minutes, or blood in urine. These are not normal side effects-they’re warning signs. Seek emergency care if you notice any of these.
Are there antidepressants that don’t affect bleeding?
Yes. Bupropion (Wellbutrin) and mirtazapine (Remeron) don’t block serotonin reuptake in platelets, so they don’t increase bleeding risk. They’re good alternatives for people with high bleeding risk, history of ulcers, or those on blood thinners. Talk to your doctor about whether one of these might work for you.
