Blood Pressure Medications: Types, Side Effects, and Safety
23 Dec, 2025High blood pressure doesn’t come with warning signs. You might feel fine, but if your numbers are consistently above 130/80 mmHg, you’re at risk for heart attack, stroke, or kidney damage. That’s why millions of people take blood pressure medication every day. But not all pills are the same. Some work better for you than others, and some come with side effects that can make you quit cold turkey. The key isn’t just lowering your number-it’s finding the right drug that works for your body, your lifestyle, and your other health conditions.
How Blood Pressure Medications Work
Blood pressure meds don’t just lower numbers-they target how your body controls pressure. Your heart pumps blood, your arteries stretch and recoil, and your kidneys manage fluid. Different drugs interfere with these systems in different ways.
Some, like thiazide diuretics, make you pee out extra salt and water. Less fluid means less pressure on your artery walls. Others, like ACE inhibitors and ARBs, block hormones that tighten blood vessels. Calcium channel blockers relax the muscles in your arteries. Beta-blockers slow your heart rate and reduce its force. Each class has a unique job, and your doctor picks based on what’s causing your high pressure-and what other health problems you have.
Common Classes of Blood Pressure Medications
There are six main types of blood pressure drugs used today, each with clear strengths and limits.
- Thiazide diuretics (like hydrochlorothiazide): First choice for most people. Cheap, effective, and proven to reduce heart attacks and strokes over time. Used in over 60% of initial prescriptions.
- Calcium channel blockers (like amlodipine): Great for older adults and Black patients. They relax arteries without affecting the heart’s rhythm too much. Often used when diuretics aren’t enough.
- ACE inhibitors (like lisinopril): Best for people with diabetes, kidney disease, or heart failure. They protect your kidneys while lowering pressure.
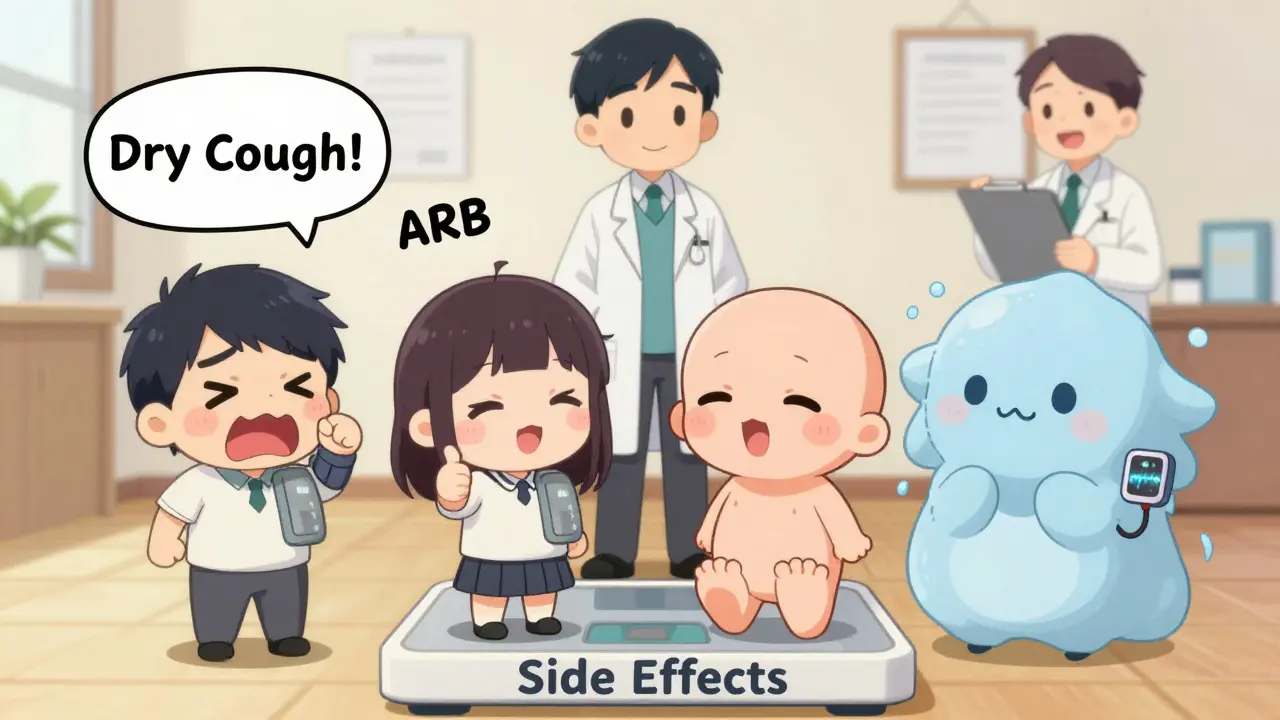
- ARBs (like losartan): Similar to ACE inhibitors but without the dry cough. Often used when someone can’t tolerate ACE drugs.
- Beta-blockers (like metoprolol): Not first-line for most, but essential after a heart attack or for those with heart failure or fast heart rhythms.
- Alpha-blockers and central agonists (like doxazosin, clonidine): Used less often. Usually added when other drugs fail, especially in resistant cases.
According to the American Heart Association, about 70% of people need two or more of these drugs to reach their goal. That’s normal-not a failure. Combination pills (like lisinopril + hydrochlorothiazide) make it easier to stick with treatment.
Side Effects You Should Know
Side effects are why so many people stop taking their meds. About half quit within a year. But not all side effects are equal. Some are annoying. Others are dangerous.
ACE inhibitors cause a dry, hacking cough in 10-20% of users. It’s not an allergy-it’s a chemical reaction. If it’s bad, switching to an ARB usually fixes it. But both ACE inhibitors and ARBs can raise potassium to dangerous levels, especially in people with kidney disease. That’s why your doctor checks your blood regularly.
Calcium channel blockers like amlodipine often cause swollen ankles, dizziness, or flushing. It’s not serious for most, but it can be embarrassing. Some people get gum swelling-gingival hyperplasia-which requires better dental care.
Diuretics can drop potassium too low, leading to muscle cramps or irregular heartbeat. They also make you pee more, which can disrupt sleep. And they can trigger gout flare-ups in people who are prone.
Beta-blockers can make you feel tired, cold, or sluggish. Diabetics need to be careful-these drugs hide the warning signs of low blood sugar, like shaking or a fast heartbeat. That’s risky if you’re on insulin.
Alpha-blockers can cause a sudden drop in blood pressure when standing up-orthostatic hypotension. That increases fall risk, especially in older adults. Taking them at bedtime helps.
None of these side effects happen to everyone. But if you notice something new after starting a new pill, don’t ignore it. Talk to your doctor. There’s almost always another option.
Safety Rules and Drug Interactions
Some combinations can be dangerous. Mixing ACE inhibitors and ARBs together sounds logical-but it doesn’t help more, and it raises your risk of kidney failure and deadly high potassium. Never do this unless your doctor specifically says so.
Nonsteroidal anti-inflammatory drugs (NSAIDs) like ibuprofen or naproxen can cancel out your blood pressure meds and damage your kidneys, especially if you’re on diuretics or ACE inhibitors. If you need pain relief, acetaminophen is safer.
Alcohol can make any blood pressure drug work too well. One drink might send your pressure crashing, especially if you’re on beta-blockers or diuretics. Limit alcohol, and never drink on an empty stomach if you’re on these meds.
Some herbs and supplements interfere too. Licorice root raises blood pressure. St. John’s wort can reduce the effect of some calcium channel blockers. Always tell your doctor what vitamins or herbal products you take.
Special Populations: Pregnancy, Seniors, and More
Pregnant women can’t take ACE inhibitors, ARBs, or direct renin inhibitors-they cause serious birth defects. Safe options include methyldopa and labetalol, which have been used for decades without harm to the baby.
Older adults are more sensitive to blood pressure drugs. A dose that works for a 40-year-old might knock a 75-year-old off their feet. Doctors start low and go slow. Orthostatic hypotension is a big concern-falls can break hips and end independence.
Black patients often respond better to diuretics and calcium channel blockers than to ACE inhibitors or beta-blockers. That’s not about race-it’s about biology. Studies show differences in how the body handles salt and hormones across populations. Guidelines reflect this.
People with diabetes need kidney protection. ACE inhibitors and ARBs are first choice here because they slow kidney damage, even if blood pressure is only slightly high. That’s why your doctor might prescribe them even if your pressure is 135/85.

How to Take Your Medication Right
Medication adherence is the biggest challenge in treating high blood pressure. You won’t feel better. You won’t feel worse. But your risk of stroke drops 40% if you take your pills daily.
Here’s how to stay on track:
- Take your pill at the same time every day-link it to brushing your teeth or eating breakfast.
- Use a pill organizer. A weekly box with morning/evening slots cuts mistakes by 50%.
- Set phone reminders. Apps like Medisafe or MyTherapy have proven to improve adherence.
- Don’t skip doses because you feel fine. Hypertension is silent by design.
- Never stop suddenly. Stopping beta-blockers cold turkey can cause rebound high pressure or even a heart attack.
If you’re struggling with side effects, don’t quit. Talk to your doctor. Maybe you need a different drug, a lower dose, or a combination pill that reduces the number of pills you take.
What’s Next? Personalized Treatment and New Research
The future of blood pressure treatment is personal. Right now, doctors guess which drug will work based on age, race, and comorbidities. But research is moving toward genetics.
Early studies suggest your DNA can predict how well you respond to beta-blockers or ACE inhibitors. In five to ten years, a simple blood test might tell your doctor which drug to start with-no trial and error.
Combination pills are getting smarter too. New versions combine three drugs in one tablet, making it easier to stick with treatment. Digital tools are helping: smart blood pressure cuffs that sync to your phone and alert your doctor if numbers spike.
For people with resistant hypertension (pressure that won’t drop despite three drugs), new devices that stimulate nerves to lower pressure are in clinical trials. But for now, the best tools are still the old ones-diuretics, calcium blockers, ACE inhibitors-used wisely.
High blood pressure isn’t a life sentence. It’s a manageable condition. The right drug, taken consistently, can give you decades of healthy life. But only if you know what you’re taking, why it matters, and what to watch for.
Can I stop taking blood pressure medication if my numbers are normal?
No, not without your doctor’s guidance. Normal numbers mean the medication is working-not that your condition is cured. Stopping suddenly can cause your pressure to rebound higher than before, increasing your risk of stroke or heart attack. Some people can reduce or stop meds after major lifestyle changes, but only under close medical supervision.
Which blood pressure medication has the least side effects?
There’s no single answer. Thiazide diuretics like hydrochlorothiazide are generally well-tolerated and have the most long-term safety data. But side effects vary by person. Amlodipine (a calcium channel blocker) often causes less fatigue than beta-blockers, and ARBs avoid the cough of ACE inhibitors. The best choice is the one that works for your body with the fewest bothersome effects.
Do blood pressure meds damage your kidneys?
Most don’t-they protect your kidneys. ACE inhibitors and ARBs are actually used to slow kidney damage in people with diabetes or proteinuria. But if you’re on multiple drugs (like diuretics + ACE inhibitors) and take NSAIDs like ibuprofen, you can risk kidney injury. Regular blood tests for creatinine and potassium help catch problems early.
Why do I need two or more blood pressure pills?
High blood pressure has multiple causes: stiff arteries, excess fluid, overactive nerves. One drug usually can’t fix all of them. Combining two or more from different classes works better than increasing the dose of one. Studies show combination therapy gets more people to their target pressure faster and with fewer side effects than doubling a single drug.
Are natural remedies safer than blood pressure meds?
No. While diet, exercise, and reducing salt help, they rarely lower pressure enough on their own for people with stage 1 or 2 hypertension. Supplements like garlic, hibiscus tea, or magnesium may help a little, but they’re not replacements for proven medications. Relying on them alone can put you at serious risk. Always discuss supplements with your doctor-they can interact with your meds.
What to Do Next
If you’re on blood pressure medication, schedule a check-up. Ask: Is this the right drug for me? Are my side effects manageable? Do I need a blood test? If you’re not on meds yet but your pressure is high, don’t wait. Start with lifestyle changes-but don’t assume they’ll be enough. Talk to your doctor about whether medication is needed.
High blood pressure doesn’t care if you feel fine. But you can take control. Know your drugs. Know your risks. Stick with your plan. Your future heart will thank you.
