Dietary Supplement-Drug Interactions: What You Need to Know for Safety
4 Dec, 2025Every year, millions of people in the U.S. take dietary supplements - vitamins, herbs, minerals, amino acids - thinking they’re harmless. After all, they’re sold on store shelves next to cereal and protein bars. But what if that daily turmeric capsule or green tea extract is quietly messing with your blood pressure medication, antidepressant, or blood thinner? The truth is, supplement-drug interactions are more common - and more dangerous - than most people realize.
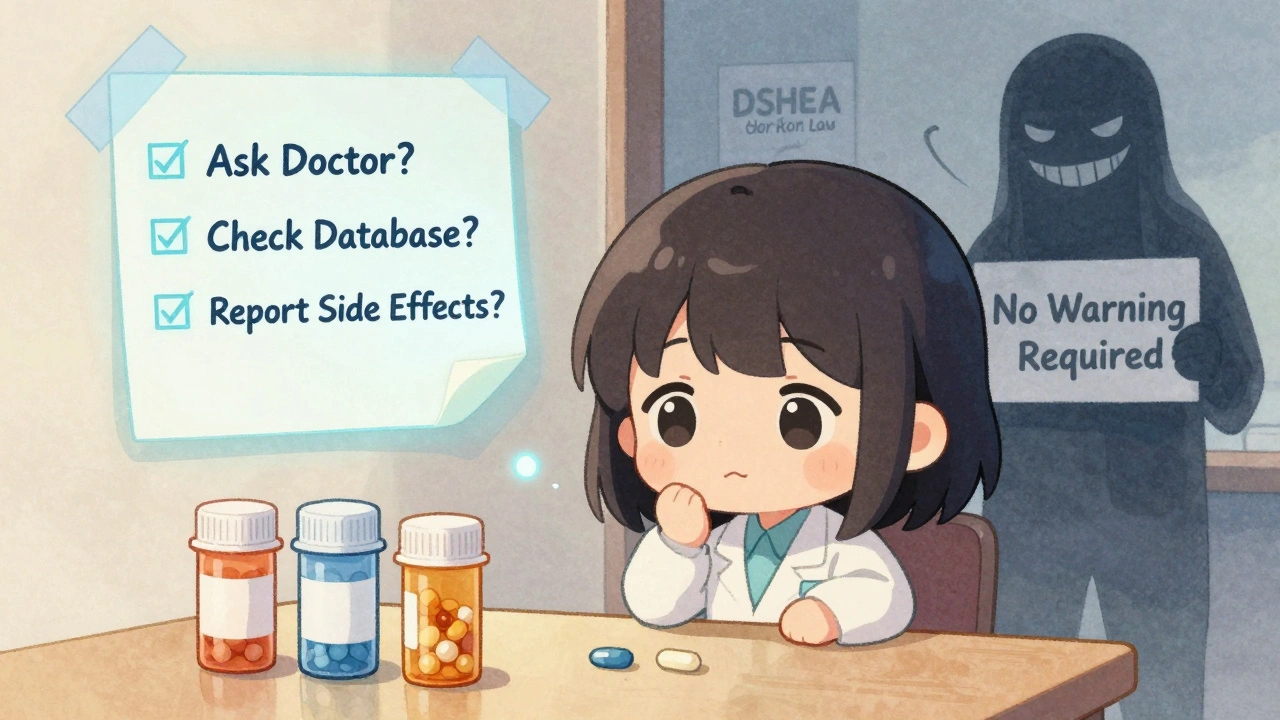
Why Supplements Aren’t Always Safe
Unlike prescription drugs, dietary supplements don’t need FDA approval before hitting the market. Under the Dietary Supplement Health and Education Act (DSHEA) of 1994, manufacturers are responsible for proving their products are safe - but the FDA can only step in after harm happens. That means thousands of supplements are sold with no real testing for how they react with medications. This gap creates a hidden risk. A 2023 study found that 78% of supplement labels don’t mention any drug interaction warnings - even when science shows clear danger. Meanwhile, 77% of U.S. adults take at least one supplement. For older adults, that number jumps to 85%, and many are on four or five prescription drugs. The mix? A ticking time bomb.How Interactions Actually Happen
There are two main ways supplements interfere with drugs:- Pharmacokinetic interactions: These change how your body absorbs, breaks down, or gets rid of a drug. Think of it like traffic on a highway - supplements can block the exit, speed up the flow, or jam the entrance.
- Pharmacodynamic interactions: These change how the drug works in your body. One might make the drug stronger. Another might cancel it out completely.
Top 5 High-Risk Supplements and Their Dangerous Partners
Not all supplements are equal. Some carry far more risk than others. Here are the most dangerous combinations based on clinical reports and FDA data:- St. John’s wort + antidepressants, birth control, or immunosuppressants: Can cause serotonin syndrome, organ rejection, or unplanned pregnancy. It’s the most common cause of serious supplement-drug interactions.
- Warfarin + ginkgo biloba, vitamin K, or green tea extract: Ginkgo can spike INR levels above 6.5 (normal is 2-3), leading to uncontrolled bleeding. Vitamin K directly fights warfarin’s effect, making blood clots more likely.
- Magnesium antacids + antibiotics like ciprofloxacin or levofloxacin: Magnesium binds to these drugs in the gut, cutting absorption by up to 90%. The antibiotic becomes useless.
- Caution with calcium + levothyroxine (thyroid meds): Calcium can block up to half the absorption of thyroid hormone. Taking them together means your thyroid levels stay low - even if you’re taking the right dose.
- CBD oil + clobazam, statins, or blood thinners: CBD slows down liver enzymes that break down these drugs. One study found it boosted clobazam levels by up to 500%, increasing drowsiness and risk of overdose.

Herbs vs. Vitamins: Which Are Riskier?
You might assume vitamins are safer. But that’s not always true. Here’s how the risks break down:| Supplement Type | High-Risk Examples | Interaction Likelihood | Common Drug Partners |
|---|---|---|---|
| Herbal Supplements | St. John’s wort, goldenseal, ginkgo, black cohosh | High | Warfarin, SSRIs, blood pressure meds, transplant drugs |
| Vitamins | Vitamin K, vitamin E, vitamin D | Moderate | Warfarin (K), aspirin (E), calcium (D) |
| Minerals | Magnesium, calcium, iron | Moderate to High | Antibiotics, thyroid meds, osteoporosis drugs |
| Amino Acids & Enzymes | Tryptophan, bromelain | Low to Moderate | Antidepressants, blood thinners |
Why People Don’t Tell Their Doctors
If you’re taking supplements, you’re probably not telling your doctor. A 2022 survey found that 68% of users never mention them during medical visits. Why?- “My doctor doesn’t know anything about supplements anyway.” - Reddit user, 2022
- “I think they’re safe because they’re natural.”
- “I didn’t think it mattered.”
What You Can Do Right Now
You don’t need to stop taking supplements. But you do need to take control. Here’s how:- Make a list. Write down every supplement you take - including brand name, dosage, and how often. Don’t forget “natural” teas, powders, or gummies.
- Ask your doctor. Don’t say, “Do you know about supplements?” Say: “I’m taking turmeric, fish oil, and a multivitamin. Could any of these interfere with my blood pressure pill or statin?”
- Check your meds. Use free tools like the NIH’s LiverTox database or the Natural Medicines Database (available through many hospital libraries).
- Watch for warning signs. Unexplained bruising, dizziness, fatigue, confusion, or sudden changes in mood or blood pressure could mean an interaction.
- Report bad experiences. If you get sick after starting a supplement, report it to the FDA’s MedWatch program. Your report helps protect others.
The Bigger Picture: Why the System Is Broken
The FDA can’t recall a dangerous supplement unless it causes harm - and even then, most cases go unreported. The Government Accountability Office estimates the FDA catches less than 1% of actual adverse events. Meanwhile, the supplement market is booming - projected to hit $82 billion by 2028. Companies aren’t required to test for interactions. Only 12% of major manufacturers do. Dr. Pieter Cohen from Harvard calls it a “public health failure.” He points to red yeast rice - sold as a “natural” cholesterol remedy - that often contains hidden lovastatin, a prescription drug. When taken with gemfibrozil, it caused muscle breakdown (rhabdomyolysis) and kidney failure. The product wasn’t recalled. It was just pulled from one retailer after complaints.What’s Changing - and What’s Next
There’s movement. In 2023, Congress proposed the Dietary Supplement Labeling Act, which would require interaction warnings on high-risk products. The NCCIH has invested $15.7 million into research by 2025, focusing on older adults and heart patients. New interaction data is being added to databases - including how CBD affects seizure meds. But until supplements are held to the same safety standards as drugs, the risk stays high. The American Medical Association has pushed for DSHEA reform since 2015. So far, little has changed.Final Thought: Natural Doesn’t Mean Safe
Just because something comes from a plant, a mineral, or a bottle labeled “all-natural” doesn’t mean it’s harmless. Supplements aren’t candy. They’re active substances - and they can interact with your medications in ways that are silent, serious, and sometimes deadly. The best protection isn’t fear. It’s awareness. Know what you’re taking. Talk to your doctor. And never assume your supplement is too small to matter.Can I take vitamin D with my blood pressure medication?
Generally, yes - vitamin D doesn’t directly interfere with most blood pressure drugs. But if you’re taking calcium supplements along with vitamin D, and you’re on a diuretic like hydrochlorothiazide, you could develop high calcium levels. Always check with your doctor, especially if you have kidney issues.
Is St. John’s wort safe if I’m not on any meds?
Even if you’re not on medication now, it’s risky. St. John’s wort can cause side effects like anxiety, dizziness, and increased sun sensitivity. It also stays in your system for days. If you start a new prescription later - even something as simple as an antibiotic or birth control - you could trigger a dangerous interaction. It’s safer to avoid it unless under medical supervision.
Why don’t supplement labels warn about drug interactions?
Because the law doesn’t require it. Under DSHEA, supplement makers don’t need to prove safety or test for interactions before selling. Warning labels are voluntary. Only a handful of brands - mostly larger, science-backed ones - include them. Most don’t, even when the science is clear.
Can I take fish oil with warfarin?
Fish oil can slightly increase bleeding risk, especially at high doses (over 3 grams per day). If you’re on warfarin, your INR should be monitored more closely when starting fish oil. Most doctors say it’s okay at lower doses, but only if your blood levels are checked regularly. Don’t start it without talking to your provider.
Are there any supplements that are always safe?
There’s no such thing as “always safe.” Even a simple multivitamin can contain vitamin K, which interferes with warfarin. Or calcium, which blocks thyroid meds. The safest approach is to assume every supplement has the potential to interact - and always check with your doctor or pharmacist before starting anything new.

Stephanie Bodde
December 4, 2025 AT 14:31Yesss!! This is so important 🙌 I took turmeric for months without telling my doc and then started feeling dizzy-turned out it was messing with my blood pressure med. Never again. Always tell your provider, even if it’s just a ‘natural’ gummy. Your health isn’t a gamble.
Philip Kristy Wijaya
December 5, 2025 AT 21:02Let me be clear the FDA is a corrupt corporate puppet regime and the entire supplement industry is a scam orchestrated by Big Pharma to keep you dependent on their patented chemicals while they profit from your ignorance. Natural remedies have been used for millennia and now they want to criminalize your right to choose what goes into your body. Wake up sheeple.
Jennifer Patrician
December 6, 2025 AT 00:17St John's Wort is definitely a government mind control agent disguised as a herbal remedy. I read on a forum that it's used to suppress immune responses so people don't notice when the vaccines start working. And don't even get me started on CBD-Big Pharma bought out all the labs that proved it cured cancer. They don't want you healthy. They want you on pills forever.
Mellissa Landrum
December 7, 2025 AT 05:53lol so the government lets you buy poison but not weed?? classic. i took ginkgo with my blood thinner and i was fine. my aunt died from lisinopril and no one says anything about that. natural = safe. chemtrails = real. also my cat takes ashwagandha and she's 19. so there.
Mark Curry
December 8, 2025 AT 19:55It’s interesting how we treat food-derived substances as harmless while pharmaceuticals are seen as inherently dangerous. But both are chemicals. The real issue isn’t supplements or drugs-it’s the lack of transparency and education. We need better labeling, yes, but also better dialogue between patients and providers. Maybe then we’d stop treating health like a DIY project.
Jimmy Jude
December 8, 2025 AT 23:05Let me tell you about the time I almost died because I took vitamin D with my thyroid med and didn’t know. My doctor didn’t ask. The pharmacist didn’t warn me. The label said ‘all natural’ so I thought it was safe. Turns out my body was slowly shutting down. I had to be hospitalized. Now I only take what my spiritual healer recommends. And I don’t trust anyone who says ‘science’ without saying ‘energy’ first.
Mark Ziegenbein
December 10, 2025 AT 18:36The regulatory framework governing dietary supplements in the United States is fundamentally incompatible with the principles of evidence-based pharmacology. The DSHEA of 1994 established a premarket exemption that effectively delegitimizes the FDA's capacity to ensure public safety. This is not merely a policy gap-it is a structural failure of governance that has enabled the commodification of pseudoscientific claims under the guise of consumer autonomy. The result is a public health crisis of cascading iatrogenic consequences.
Rupa DasGupta
December 11, 2025 AT 23:05OMG I just started taking magnesium and now I'm crying all the time?? Is it the supplement or is it the moon phase?? I think it's both. Also my mom says vitamin C cures everything but my cousin took it with chemo and now he's in a coma?? So I don't know anymore. I'm just gonna drink lemon water and pray 🙏
an mo
December 12, 2025 AT 18:00Based on the 2023 FDA Adverse Event Reporting System dataset, herbal supplements account for 68.3% of Class I recalls involving polypharmacy patients over 65. The pharmacokinetic interference profile of St. John’s wort is particularly concerning due to CYP3A4 and P-gp induction. You cannot generalize risk across supplement classes. Risk stratification requires pharmacogenomic context. Stop treating this like a blog post and start treating it like clinical science.
aditya dixit
December 14, 2025 AT 03:08I’ve been taking ashwagandha for anxiety and fish oil for heart health for 3 years. My doctor knows. We check my INR every 6 weeks. I don’t assume safety-I check. Knowledge isn’t fear. It’s responsibility. And yes, I’ve told my sister, my neighbor, and my yoga teacher. Small acts, big ripples.
Lynette Myles
December 14, 2025 AT 16:58St. John’s wort + SSRIs = serotonin syndrome. End of story. No debate. No ‘natural’ excuse. Just death.
Annie Grajewski
December 16, 2025 AT 16:11Oh wow you mean that ‘natural’ energy gummy I’ve been eating since 2020 has vitamin K in it?? And I’m on warfarin?? Oh no wait I’m fine I just had a stroke last week so it’s probably fine. Jk jk 😘 maybe I’ll just start taking ‘detox tea’ next. I heard it fixes everything. Even cancer. And my ex.
ashlie perry
December 17, 2025 AT 15:25They’re lying about CBD. It’s not for anxiety. It’s for mind control. The FDA knows. The WHO knows. But they won’t say it because they’re paid by the pharmaceutical companies who make the real drugs. I’ve been off all meds since 2021 and I’m healthier than ever. My blood pressure is perfect. My skin glows. My dog even smells better. It’s not luck. It’s truth.
Juliet Morgan
December 17, 2025 AT 19:37I used to think supplements were harmless too… until my grandma ended up in the ER after mixing ginkgo with her blood thinner. She didn’t even know it was dangerous. I started a little list on my fridge: ‘Supplements + Meds = Check with Dr.’ Now my whole family does it. It’s not scary. It’s just smart.
William Chin
December 19, 2025 AT 19:06As a licensed pharmacist with over seventeen years of clinical experience in geriatric pharmacotherapy, I must emphasize that the absence of labeling requirements under DSHEA constitutes a gross dereliction of duty by regulatory authorities. The conflation of ‘natural’ with ‘safe’ is not merely a semantic error-it is a lethal cognitive bias that results in preventable morbidity and mortality. I routinely counsel patients on supplement-drug interactions, yet only 12% of my colleagues initiate the conversation. This is not patient negligence. This is systemic negligence.