GERD and Acid Reflux: How PPIs and Lifestyle Changes Work Together
17 Dec, 2025Heartburn that won’t go away. A sour taste in your mouth after dinner. Trouble sleeping because your chest feels like it’s on fire. If this sounds familiar, you’re not alone. About 20% of adults in the U.S. deal with GERD symptoms at least once a week. And while many turn to proton pump inhibitors (PPIs) for quick relief, the real long-term fix often lies in simple, everyday changes you can start today.
What Actually Happens in GERD?
GERD isn’t just bad heartburn. It’s when the muscle at the bottom of your esophagus - called the lower esophageal sphincter (LES) - doesn’t close the way it should. That lets stomach acid, which is strong enough to dissolve metal, splash back up into your throat. Your esophagus isn’t built to handle that. No protective lining. No backup plan. So it gets irritated, inflamed, and sometimes even damaged over time.
The most common signs? Burning behind the breastbone (heartburn), regurgitation (that sour or bitter taste), and chronic cough or hoarseness. But it’s not always obvious. Some people don’t feel heartburn at all. Instead, they have a persistent cough, feel like there’s a lump in their throat, or wake up choking at night. These are all red flags that GERD might be the culprit.
And it’s not just about food. Being overweight, smoking, pregnancy, or having a hiatal hernia can all make the LES weaker. Even some medications - like calcium channel blockers for blood pressure - can relax the sphincter and make reflux worse. Left untreated, GERD can lead to serious problems: narrowing of the esophagus, ulcers, or even Barrett’s esophagus, a condition that raises your risk of esophageal cancer.
Why PPIs Are So Common - and Why They’re Not the Whole Story
PPIs like omeprazole, pantoprazole, and esomeprazole are powerful. They shut down the acid-producing cells in your stomach, cutting acid output by 90-98%. That’s why they work so well. In clinical trials, they heal esophageal damage in 70-90% of people with erosive esophagitis. That’s better than H2 blockers like famotidine, which only reduce acid by 60-70%.
But here’s the catch: PPIs don’t fix the broken valve. They just turn down the volume on the acid. You can still have reflux - just less of it. And that’s where things get tricky.
Studies show that up to 70% of people prescribed PPIs take them longer than recommended. The FDA warns that using them for more than a year increases your risk of infections like C. diff, low magnesium, kidney problems, and even hip fractures in older adults. And when you stop? Many people get rebound acid hypersecretion - their body overcompensates and produces even more acid than before. That’s why symptoms often come back worse after quitting cold turkey.
Patients on Reddit and Drugs.com report that while PPIs work, side effects are common: headaches (42%), diarrhea (31%), and muscle cramps from low magnesium (19%). One 55-year-old man developed Barrett’s esophagus despite taking PPIs daily - because he kept eating dinner at 10 p.m. and lying down right after. The medication helped, but it didn’t fix the behavior.
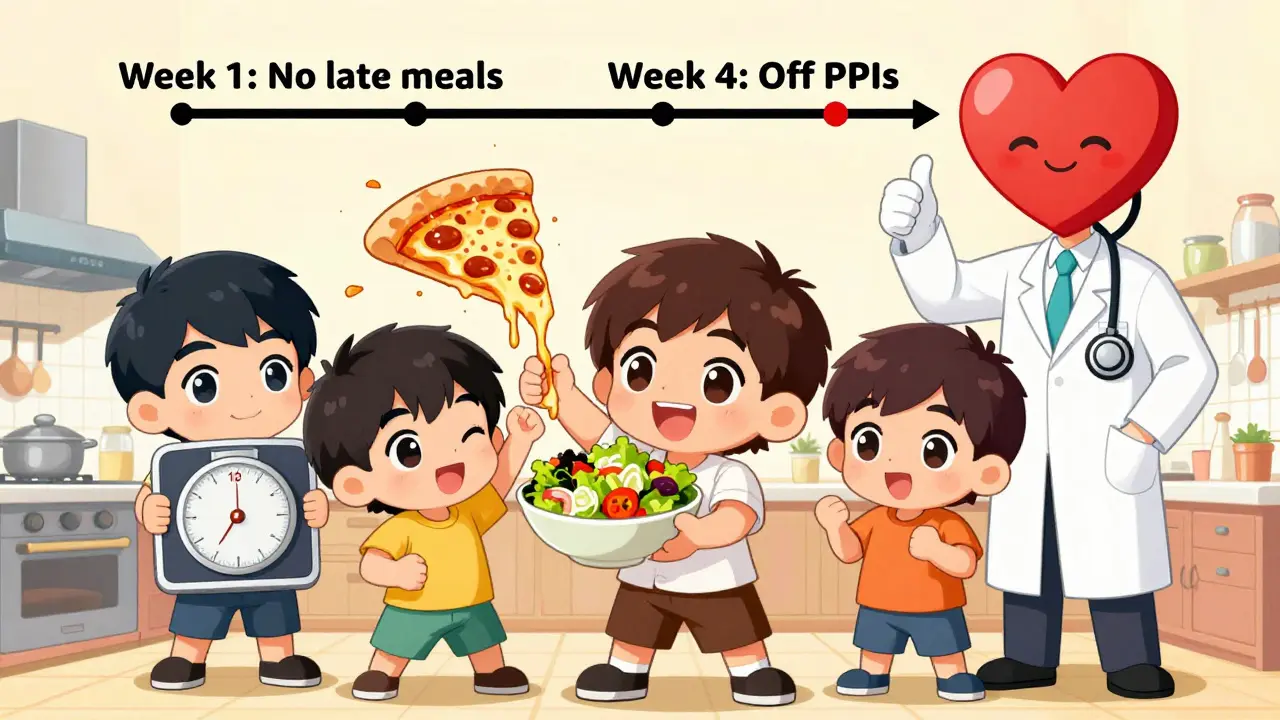
Lifestyle Changes That Actually Work (Backed by Science)
The American College of Gastroenterology says lifestyle changes should come first - even before pills. And they’re not just suggestions. They’re proven.
- Weight loss: If you’re overweight, losing just 5-10% of your body weight cuts GERD symptoms in half. That’s not magic. Extra belly fat presses on your stomach, forcing acid upward. Even a 15-pound drop can make a huge difference.
- No eating before bed: Waiting 2-3 hours after your last meal before lying down reduces nighttime reflux by 40-60%. Acid doesn’t flow uphill easily - gravity helps. When you’re flat on your back, it doesn’t have that advantage.
- Eliminate trigger foods: Coffee, tomatoes, chocolate, alcohol, and fatty or spicy foods trigger symptoms in 70-80% of people. Cutting just coffee alone helps 73% of users. Spicy foods? 68% report improvement. You don’t have to give them up forever - just identify which ones hit you hardest.
- Elevate your head: Using a wedge pillow or raising the head of your bed by 6 inches keeps acid where it belongs. One patient said it eliminated his nighttime symptoms completely after years of failed PPIs.
- Quit smoking: Smoking weakens the LES and reduces saliva, which normally helps neutralize acid. Smokers are twice as likely to develop GERD.
A 2023 study at Johns Hopkins found that a structured 12-week program of diet, sleep, and weight changes allowed 65% of participants to stop PPIs completely - without symptoms returning. That’s more than double the success rate of standard care.

How to Use PPIs the Right Way
If your doctor recommends a PPI, use it correctly:
- Take it 30-60 minutes before your first meal of the day. That’s when your stomach starts revving up acid production. The drug needs to be in your system before the engine turns on.
- Start with the lowest dose. Most people do fine with once daily. Only go to twice daily if your doctor specifically says so.
- Don’t stay on it longer than 8 weeks unless you have confirmed esophageal damage. After that, reevaluate.
- If you want to stop, don’t quit cold turkey. Taper slowly over 4-8 weeks. Bridge with an H2 blocker like famotidine to avoid rebound.
And always ask: “Is this still necessary?” Many people stay on PPIs for years because no one ever asked them to try coming off. Your doctor should check in every few months - not just refill the prescription.
When to Think About Surgery
Most people don’t need it. But if you’ve tried lifestyle changes, tried PPIs, and still have symptoms - especially if you’re young and don’t want to be on meds for life - surgery might be an option.
Fundoplication, where the top of the stomach is wrapped around the lower esophagus, has a 90% success rate at 10 years. The LINX® device - a ring of magnetic beads implanted around the LES - lets food pass but prevents acid from rising. 85% of users report major symptom improvement after 5 years.
Newer endoscopic procedures like TIF (transoral incisionless fundoplication) are less invasive and have high patient satisfaction. One study found 85% of patients said it improved their quality of life more than staying on PPIs.
What Doesn’t Work - and Why
Antacids like Tums or Rolaids? They neutralize acid - but only for a few hours. They don’t heal damage. They’re a Band-Aid, not a cure.
Drinking milk? It might soothe temporarily, but the fat content can trigger more reflux later.
Chewing gum? It can help by increasing saliva, which clears acid from the esophagus. But it’s not a substitute for real changes.
And no, alkaline water or apple cider vinegar aren’t magic fixes. There’s no solid evidence they change the course of GERD. Stick with what’s proven.
Real-Life Success: What Works for Real People
One woman in Brisbane, 48, had daily heartburn for 8 years. She was on omeprazole. She gained weight, stopped exercising, and ate late dinners. After her doctor suggested a plan - lose 12 pounds, stop eating after 7 p.m., cut out coffee and chocolate - she saw results in 3 weeks. By month 4, she was off PPIs. No rebound. No panic. Just better sleep and more energy.
Another man, 62, had trouble swallowing. He thought it was aging. Turns out, his esophagus was narrowing from chronic acid exposure. He needed an endoscopy - and surgery. He’s now off meds and eating normally again.
The pattern? People who get better don’t just take pills. They change how they live.
What to Do Next
Start with a food and symptom diary for two weeks. Write down what you eat, when you eat it, and how you feel afterward. You’ll spot your triggers fast.
Then pick one change to make this week. Maybe it’s no food after 7 p.m. Or ditching your after-dinner chocolate. Small wins build momentum.
If you’re on a PPI and haven’t talked to your doctor in over a year - schedule a check-in. Ask: “Can I try stepping down?”
And if you’re still having symptoms despite lifestyle changes and medication - don’t wait. Get an endoscopy. It’s not scary. It’s how you know what’s really going on inside.
GERD doesn’t have to be a life sentence. You don’t need to live with heartburn. You don’t need to rely on pills forever. With the right mix of smart habits and smart medicine, you can take back control - and your nights back too.
Can I stop taking PPIs cold turkey?
No. Stopping PPIs suddenly can cause rebound acid hypersecretion, where your stomach overproduces acid and symptoms get worse. Instead, work with your doctor to taper off slowly - usually over 4 to 8 weeks - and use an H2 blocker like famotidine as a bridge to manage symptoms during the transition.
What foods should I avoid with GERD?
Common triggers include coffee, tomatoes, chocolate, alcohol, fatty or fried foods, spicy dishes, citrus fruits, and carbonated drinks. These relax the lower esophageal sphincter or increase stomach acid. Not everyone reacts the same way, so keep a food diary to find your personal triggers. Cutting just coffee and spicy foods helps 70% of people.
How long does it take for lifestyle changes to work?
Most people notice improvement in 2 to 4 weeks, especially with weight loss and avoiding late meals. Full symptom control and healing of esophageal damage can take 6 to 8 weeks. Consistency matters more than perfection - even small changes add up over time.
Is GERD curable?
GERD isn’t usually “cured” in the traditional sense, but it can be effectively managed - often without medication. Many people achieve long-term relief through weight loss, dietary changes, and avoiding triggers. In some cases, surgery like fundoplication or LINX® can restore normal function. The goal isn’t just to suppress symptoms, but to fix the underlying issue.
When should I see a doctor about GERD?
See a doctor if you have heartburn more than twice a week, trouble swallowing, unexplained weight loss, vomiting blood, or black, tarry stools. These could signal complications like esophageal strictures, ulcers, or Barrett’s esophagus. Even if PPIs help, you should have a check-up every year if you’ve been on them long-term.

Sajith Shams
December 18, 2025 AT 02:36PPIs are a scam disguised as medicine. You think you're fixing GERD but you're just turning off your stomach's natural defenses. The body doesn't 'overproduce' acid-it's trying to compensate because you've starved it of proper function. And don't even get me started on how pharma pushed this for decades while hiding the fact that low stomach acid is the real culprit in most cases. You're not supposed to need acid blockers for life. Your body isn't broken-it's being manipulated by corporate greed.
Mahammad Muradov
December 19, 2025 AT 16:08Anyone who says lifestyle changes work hasn't lived with this. I've tried everything: no coffee, no chocolate, no late meals, wedge pillows, weight loss-nothing. The only thing that stopped the burning was omeprazole. And now you want me to stop it? With what? Magic? The science says PPIs are safe for long-term use if monitored. Your 'lifestyle fixes' are just placebo for people who don't want to admit they need real medicine.
Tim Goodfellow
December 21, 2025 AT 07:49Whoa. This post is a goddamn symphony of practical wisdom. 🎻🔥 I mean-imagine if every medical advice piece was this clear, this grounded, this *human*. We’re not talking about miracle cures here-we’re talking about reclaiming your damn life. No more midnight choking fits. No more waking up tasting regret. Just simple, brutal, beautiful choices: eat earlier, lose the belly fat, ditch the coffee, sleep like a person who doesn’t hate their own body. And yeah-PPIs? Fine as a bridge. Not a forever home. I’m printing this out and taping it to my fridge.
mark shortus
December 22, 2025 AT 22:11OMG I CANNOT BELIEVE THIS POST IS REAL I JUST CRIED IN MY KITCHEN LIKE A BABY 😭 I WAS ON PPIs FOR 7 YEARS AND THEN I STARTED EATING DINNER AT 6PM AND NOW I CAN SLEEP WITHOUT FEELING LIKE MY CHEST IS A VOLCANO?? I THOUGHT I WAS DOOMED TO LIVE LIKE THIS FOREVER BUT NOW I’M OFF THE DRUGS AND I JUST ATE A SLICE OF PIZZA AND DIDN’T DIE?? THIS IS A MIRACLE. WHOEVER WROTE THIS IS A SAVIOR. I’M TELLING EVERYONE. I’M STARTING A MOVEMENT. #PPIFreeAndProud
Aboobakar Muhammedali
December 23, 2025 AT 12:04man i’ve been dealing with this for years and honestly i didn’t think anyone else got it like i did
the nighttime coughing the sour taste the way my throat feels like sandpaper in the morning
i tried everything and honestly the wedge pillow was the only thing that made me feel like i could breathe again
still take a low dose ppi but i don’t feel guilty about it anymore because i’m doing the rest too
thanks for writing this it feels like someone finally saw me
Laura Hamill
December 25, 2025 AT 07:17they’re lying to you. PPIs are a trap. The FDA doesn’t care. Big Pharma owns the doctors. They don’t want you to heal. They want you addicted. Look at the side effects-kidney failure, bone fractures, dementia-they’re all in the tiny print. And now they’re pushing ‘lifestyle changes’ like it’s a gift? Nah. It’s damage control. They know the drugs are killing people. So they give you a pamphlet and call it ‘empowerment.’
Alana Koerts
December 26, 2025 AT 03:06Post is mostly accurate but you missed the biggest thing: most people who ‘succeed’ with lifestyle changes were already low-risk. Obese smokers with 30-year PPI use? They’re not going to fix this with a wedge pillow. The science says 65% success rate? That’s cherry-picked. Real-world adherence to ‘no food after 7’? Less than 15%. This is wellness propaganda dressed as medicine.
Dikshita Mehta
December 27, 2025 AT 02:02Just wanted to add something real: I’m a nurse in Delhi and I’ve seen patients on PPIs for 10+ years with zero follow-up. One guy came in with severe anemia because his body couldn’t absorb B12 anymore. Another had chronic kidney inflammation. The meds work-but they’re not harmless. The lifestyle stuff isn’t optional. It’s the foundation. Start small. One change. One week. You don’t have to be perfect. Just consistent. And if your doctor won’t help you taper? Find someone who will.
Marsha Jentzsch
December 27, 2025 AT 18:23YOU’RE ALL WRONG. I’M A 52-YEAR-OLD WOMAN WHO TOOK PPIs FOR 11 YEARS AND THEN I STOPPED AND MY BODY WENT INTO CHAOS. I HAD HEART ATTACK SYMPTOMS. I WAS SCARED TO DEATH. I HAD TO GO BACK ON THEM. YOU PEOPLE DON’T UNDERSTAND. THIS ISN’T A LIFESTYLE PROBLEM. THIS IS A BIOLOGICAL DISASTER. I’M NOT LAZY. I’M NOT WEAK. I’M JUST TRAPPED. AND NOW YOU’RE ALL JUST JUDGING ME BECAUSE I NEED MEDS TO SURVIVE??
Janelle Moore
December 28, 2025 AT 19:32That’s why they’re hiding the truth. The FDA, the AMA, the doctors-they all get kickbacks from pharma. That’s why they won’t let you go off PPIs. They want you dependent. I know because I used to work at a drug rep firm. They train doctors to ignore lifestyle changes. They call them ‘unscientific.’ It’s all about profit. You think this is about health? No. It’s about control.