How to Measure Children’s Medication Doses Correctly at Home
9 Dec, 2025Getting the right dose of medicine for your child isn’t just about following the label-it’s about avoiding mistakes that can make your child sick or even put them in danger. Every year, thousands of children end up in emergency rooms because someone gave them too much-or too little-medicine. And the most common cause? Using the wrong tool to measure liquid medication. A kitchen spoon. A dosing cup with confusing markings. Even a dropper used incorrectly. These aren’t rare mistakes. They’re everyday ones. The good news? With the right tools and a few simple habits, you can cut the risk of error by more than half.
Why Measuring Medicine for Kids Is So Different
Children aren’t small adults. Their bodies process medicine differently, and even a tiny mistake can have big consequences. A dose that’s 10% too high might cause drowsiness. A dose that’s 100% too high? It could stop their breathing. That’s why the American Academy of Pediatrics and the CDC both say: milliliters only. No teaspoons. No tablespoons. No guessing.
Here’s the scary part: studies show that 7 in 10 parents mismeasure liquid medicine at least once. Why? Because most dosing tools still show both milliliters (mL) and teaspoons (tsp), and people mix them up. Confusing 0.5 mL with 5 mL isn’t just a slip-it’s a tenfold overdose. That’s the difference between a safe dose and a life-threatening one.
And it’s not just about the numbers. Many parents don’t realize that liquid medicines need to be shaken before use. If you don’t shake an antibiotic suspension properly, you might give your child only half the dose they need. That doesn’t just mean the infection won’t clear-it can make bacteria stronger, leading to longer illness and harder-to-treat infections later.
The Right Tools for the Job
Not all measuring tools are created equal. Here’s what works-and what doesn’t.
- Oral syringes (1-10 mL): These are the gold standard, especially for doses under 5 mL. They’re precise, easy to control, and let you slowly deliver the medicine into your child’s cheek, reducing spit-out rates. Studies show they’re 94% accurate.
- Dosing cups (5-30 mL): Better than spoons, but still error-prone. For doses under 5 mL, error rates jump to nearly 70%. Only use these if your child is old enough to drink from a cup without spilling.
- Droppers (1-2 mL): Fine for babies, but hard to read accurately. Only use if the medicine comes with one and it’s clearly marked in mL.
- Medication spoons: Only if labeled in mL and designed for medicine. Kitchen spoons? Never. A regular kitchen teaspoon can hold anywhere from 3.9 to 7.3 mL-way off from the standard 5 mL.
The CDC and AAP agree: if the dose is less than 5 mL, use an oral syringe. Always. No exceptions. Even if the pharmacy gives you a cup, ask for a syringe. Most will give you one for free.
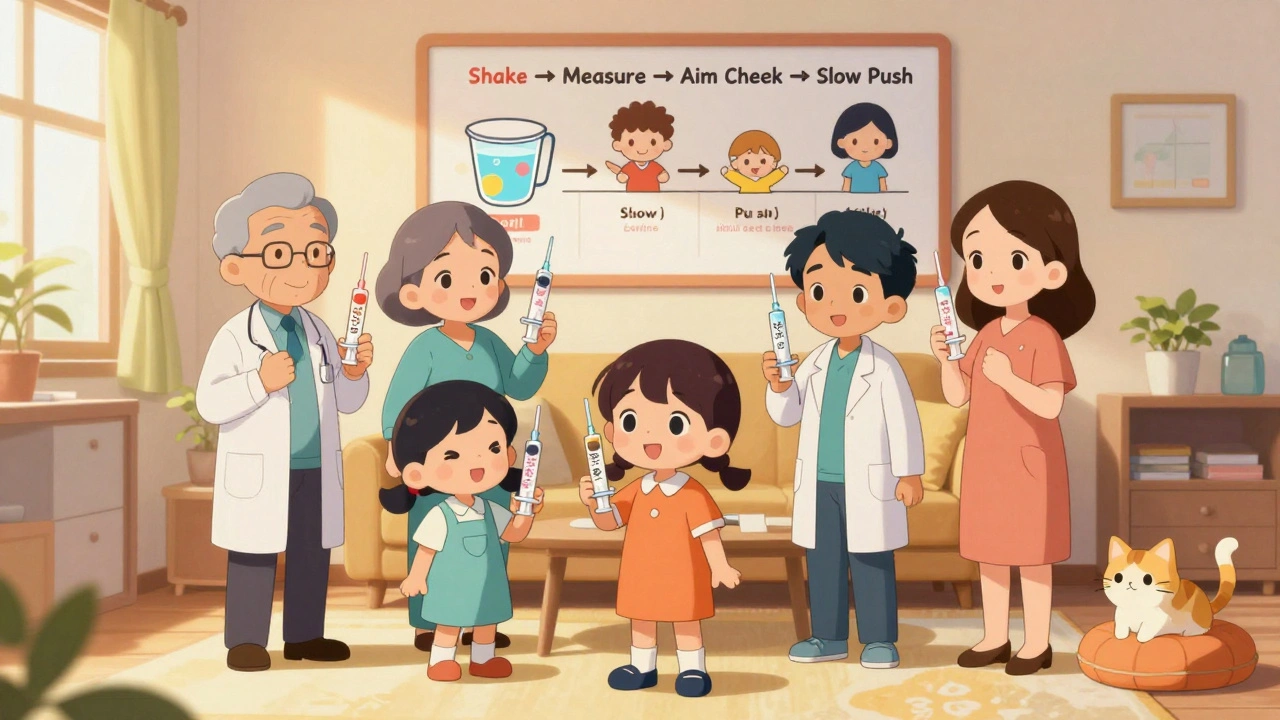
How to Measure Accurately-Step by Step
Here’s exactly how to get it right every time:
- Read the label. Confirm the dose is in mL. If it says “1 tsp,” ask the pharmacist to rewrite it in mL. Don’t assume.
- Use the right tool. Always use the syringe or cup that came with the medicine. Never substitute a kitchen spoon, eye dropper, or other container.
- Shake the bottle. Liquid medicines often settle. Shake well for 10-15 seconds before each dose.
- Hold the syringe vertically. Place it on a flat surface, eye level. Look straight at the markings. The medicine forms a curve (meniscus)-read the bottom of that curve.
- Draw the exact dose. Pull back the plunger slowly. If you go too far, don’t push it back. Discard it and start over.
- Give it slowly. Place the tip of the syringe inside your child’s cheek, not at the front of the mouth. Gently push the plunger to let the medicine drip slowly. This reduces gagging and spitting.
- Record the dose. Write it down or mark your calendar. If more than one person gives medicine, this prevents double-dosing.
Weight-Based Dosing: What You Need to Know
Many children’s medications are dosed by weight-not age. That means you need to know your child’s weight in kilograms (kg), not pounds.
Here’s how to convert: Divide pounds by 2.2. For example, a 22-pound child is 10 kg (22 ÷ 2.2 = 10).
Then check the prescription: “40 mg/kg/day” means 40 milligrams per kilogram of body weight, each day. If the dose is split into two doses, divide that number in half.
Example: Amoxicillin for a 22-lb (10 kg) child with an ear infection, at 40 mg/kg/day in two doses:
- 40 mg × 10 kg = 400 mg per day
- 400 mg ÷ 2 = 200 mg per dose
- Medicine concentration: 400 mg per 5 mL
- So: 200 mg = 2.5 mL per dose
If you’re unsure, ask your pharmacist to show you the math. Write it down. Keep it on your fridge.

Common Mistakes (and How to Avoid Them)
Parents make the same mistakes over and over. Here’s how to sidestep them:
- Mistake: Using a kitchen spoon. Solution: Throw it out. Buy a set of oral syringes online or ask your pharmacy for one.
- Mistake: Measuring medicine in the dark. Solution: Always measure in good light. Use a flashlight if needed.
- Mistake: Giving medicine without shaking the bottle. Solution: Shake every time. Set a reminder on your phone.
- Mistake: Giving two doses too close together. Solution: Use a dosing chart. Mark times clearly: 8 a.m., 8 p.m. Stick to it.
- Mistake: Assuming all pharmacies label correctly. Solution: Always double-check the label. If it says “tsp,” ask them to rewrite it in mL.
What to Do When Your Child Refuses Medicine
It’s not just about measuring-it’s about getting the medicine in. About two-thirds of parents report their child spits out or refuses liquid medicine.
Try these proven tricks:
- Use a syringe to squirt the medicine into the side of the mouth, near the cheek. Avoid the tongue-it triggers the gag reflex.
- Offer a small sip of water or juice right after. Avoid milk-it can interfere with some antibiotics.
- Mix the medicine with a small amount of applesauce, yogurt, or juice. Check with your pharmacist first-some meds shouldn’t be mixed.
- Use flavored syrups if available. Many pharmacies offer flavoring options for free.
- Let your child hold the syringe (without the medicine) and pretend to give it to a stuffed animal. It reduces fear.
When to Call the Doctor or Pharmacist
You don’t have to figure this out alone. Call if:
- The label doesn’t list the dose in mL.
- You’re unsure how much to give based on your child’s weight.
- Your child vomits within 15 minutes of taking the medicine.
- You accidentally give too much-or too little-and aren’t sure what to do.
- You’re using medicine from a previous illness and aren’t sure if the dose is still correct.
Pharmacists are trained for this. They’ve seen it all. Don’t feel bad asking. It’s your job to be sure.
What’s Changing in Pediatric Dosing
Things are getting better. Since 2015, the percentage of pediatric liquid medicines labeled in mL only has jumped from 42% to 78%. The FDA is now pushing for a rule that would require every new pediatric liquid medicine to come with a built-in oral syringe marked in mL only.
Some hospitals are already giving out color-coded syringes-like NurtureShot-that change color when the right dose is drawn. In trials, these reduced errors by 61%. New apps from Cincinnati Children’s Hospital use your phone’s camera to guide you through dosing with augmented reality.
But progress isn’t universal. Low-income families are over three times more likely to make dosing errors-often because they don’t have access to proper tools or can’t afford to buy syringes. If you’re struggling, ask your clinic or pharmacy for help. Many have free programs.
Final Checklist Before Giving Medicine
Before you give your child any liquid medicine, run through this quick list:
- Is the dose written in mL? If not, ask for it to be rewritten.
- Am I using the tool that came with the medicine? No kitchen spoons.
- Did I shake the bottle well?
- Did I measure at eye level, reading the bottom of the meniscus?
- Am I giving the right dose for my child’s weight?
- Is this the right medicine for this illness? (Double-check the name.)
- Did I write down the time and dose?
If you answered yes to all seven, you’ve done everything right. And that’s how you keep your child safe.
Can I use a kitchen teaspoon to measure my child’s medicine?
No. A kitchen teaspoon can hold anywhere from 3.9 to 7.3 milliliters, while a standard medicine teaspoon is exactly 5 mL. That variation can lead to dangerous overdoses or underdoses. Always use a proper dosing tool like an oral syringe or dosing cup marked in milliliters.
What’s the difference between mg and mL?
Milligrams (mg) measure the amount of active drug in the medicine. Milliliters (mL) measure the volume of liquid. For example, a medicine might be labeled as 100 mg per 5 mL. That means every 5 mL of liquid contains 100 mg of the drug. Confusing mg and mL is one of the most common causes of pediatric dosing errors.
Should I always use an oral syringe for my baby?
Yes, especially for doses under 5 mL. Oral syringes are the most accurate tool for infants and toddlers. They allow you to deliver the medicine slowly into the cheek, reducing spit-out and gagging. Most pharmacies will give you one for free-just ask.
What if my child spits out the medicine?
If your child spits out the medicine within 15 minutes of giving it, you can give the full dose again. If it’s been longer than 15 minutes, don’t give another dose-wait until the next scheduled time. Always check with your pharmacist or doctor if you’re unsure.
How do I convert my child’s weight from pounds to kilograms?
Divide the weight in pounds by 2.2. For example, a child weighing 33 pounds is 15 kg (33 ÷ 2.2 = 15). This is needed to calculate correct doses for medications that are prescribed by weight (mg/kg).
Is it safe to mix medicine with food or juice?
Sometimes, yes. You can mix liquid medicine with a small amount of applesauce, yogurt, or juice to make it easier for your child to take. But always check with your pharmacist first-some medications (like antibiotics or thyroid medicine) shouldn’t be mixed with certain foods or liquids because it affects how they’re absorbed.
Why do some medicine bottles say “shake well”?
Many liquid medicines are suspensions-meaning the active drug is suspended in liquid and can sink to the bottom. If you don’t shake the bottle, the first dose you give might be too weak, and the last dose too strong. Always shake for 10-15 seconds before each use to make sure the medicine is evenly mixed.
Can I reuse an oral syringe for different medicines?
No. Never reuse an oral syringe for a different medicine without cleaning it thoroughly. Even then, it’s best to use a separate syringe for each medication to avoid cross-contamination. If you’re unsure, ask your pharmacist for a new one-most will give you extras at no cost.
What to Do Next
Start today. Go to your medicine cabinet. Find the last liquid medicine you gave your child. Look at the dosing tool. Is it an oral syringe? Is it marked in mL? If not, go to your pharmacy and ask for one. Bring your child’s weight in kilograms. Ask them to write the dose on the bottle in mL only. Take a photo of it. Save it in your phone.
Teach every caregiver-grandparents, babysitters, daycare staff-the same method. Make a simple chart: “For 22 lb child: 2.5 mL amoxicillin, twice daily, use syringe.” Tape it to the fridge.
Medication errors aren’t about being careless. They’re about confusion, lack of tools, and misinformation. You’re not alone. And you don’t have to guess. With the right tools and habits, you can give your child the right dose-every time.

Richard Eite
December 10, 2025 AT 17:18Katherine Chan
December 12, 2025 AT 11:17Philippa Barraclough
December 12, 2025 AT 19:48Tim Tinh
December 14, 2025 AT 06:01Olivia Portier
December 15, 2025 AT 00:19Jennifer Blandford
December 15, 2025 AT 12:45Brianna Black
December 17, 2025 AT 09:58Shubham Mathur
December 18, 2025 AT 00:25Ruth Witte
December 19, 2025 AT 23:20Darcie Streeter-Oxland
December 20, 2025 AT 00:16Taya Rtichsheva
December 21, 2025 AT 23:54Christian Landry
December 22, 2025 AT 06:00Sarah Gray
December 23, 2025 AT 15:55om guru
December 24, 2025 AT 07:03