How Type 2 Diabetes Relates to High Blood Pressure
13 Oct, 2025Understanding the link between type 2 diabetes and high blood pressure can feel like solving a puzzle-each piece of lifestyle, genetics, and physiology fits together to shape your health. In this article we break down the science, point out the shared culprits, and give you practical steps to keep both numbers in check.
Key Takeaways
- Type 2 diabetes and high blood pressure often appear together because they share insulin resistance, obesity, and inflammation.
- High blood pressure speeds up heart‑and‑vessel damage already caused by elevated blood sugar.
- Managing weight, reducing sodium, and staying active help control both conditions simultaneously.
- Regular monitoring of blood glucose and blood pressure lets you catch problems early.
- If lifestyle tweaks aren’t enough, medication combinations are safe and effective when guided by a health professional.
What Is Type 2 Diabetes?
Type 2 Diabetes is a chronic metabolic disorder where the body either resists the effects of insulin or doesn’t produce enough insulin to keep blood glucose levels normal. First identified as a distinct condition in the 1930s, it now affects over 460 million adults worldwide, according to the International Diabetes Federation.
Key attributes include:
- Elevated fasting glucose (>126mg/dL) or HbA1c (≥6.5%).
- Insulin resistance in muscle, liver, and fat cells.
- Gradual onset, often linked to excess body weight.
What Is High Blood Pressure?
High Blood Pressure, medically known as hypertension, describes a persistent elevation of the force that blood exerts on artery walls. The American Heart Association defines stage1 hypertension as a systolic reading of 130‑139mmHg or a diastolic reading of 80‑89mmHg.
Characteristics:
- Often symptom‑less, earning the nickname “the silent killer.”
- Can be primary (essential) or secondary to another condition.
- Long‑term high pressure damages arteries, heart, kidneys, and brain.
How They Influence Each Other
When you combine the two, the damage compounds. Insulin resistance-central to type2 diabetes-also encourages blood vessels to stiffen, making it harder for blood to flow. This stiffness raises systolic pressure. Meanwhile, high blood pressure reduces the ability of insulin‑dependent tissues to receive glucose, worsening hyperglycemia.
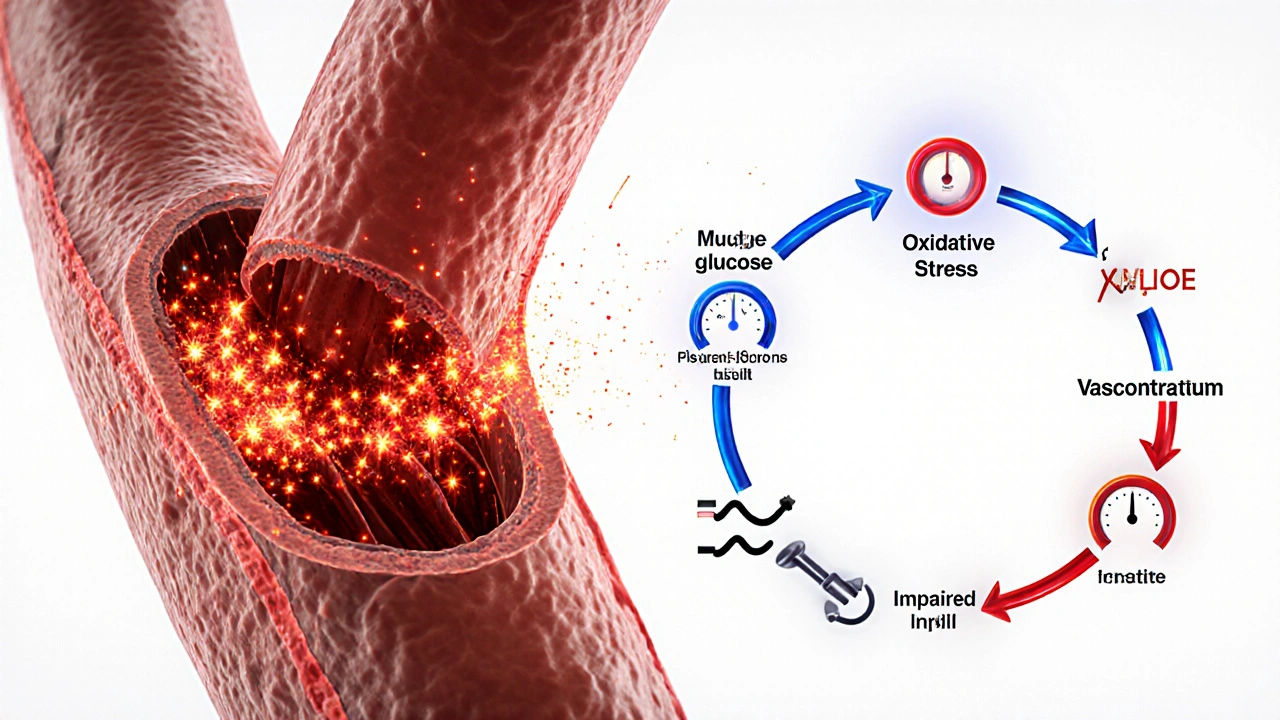
Scientific studies from 2022-2024 show that people with both conditions have a 2‑3‑fold higher risk of heart attack compared to those with just one. The physiological loop looks like this:
- Excess glucose → oxidative stress → endothelial dysfunction.
- Endothelial dysfunction → reduced nitric oxide → vasoconstriction.
- Vasoconstriction → higher blood pressure.
- Higher pressure → worsened insulin delivery → higher glucose.
Breaking any link in the chain can help the whole system recover.
Shared Risk Factors
Both conditions thrive on the same unhealthy habits. Below is a quick comparison of the most common contributors.
| Risk Factor | Impact on Diabetes | Impact on Blood Pressure |
|---|---|---|
| Obesity (especially visceral fat) | Increases insulin resistance, raises fasting glucose. | Elevates cardiac output and activates renin‑angiotensin system. |
| High Sodium Intake | Can worsen insulin resistance via fluid retention. | Directly raises extracellular fluid volume, boosting pressure. |
| Physical Inactivity | Reduces muscle glucose uptake, aggravates insulin resistance. | Leads to higher resting heart rate and arterial stiffness. |
| Chronic Stress | Elevates cortisol, spiking blood sugar. | Triggers sympathetic nervous system, raising pressure. |
| Unhealthy Diet (high sugars, saturated fats) | Feeds hyperglycemia and dyslipidemia. | Promotes atherosclerosis, narrowing vessels. |
Notice how many of these are modifiable. That’s good news because you can attack both problems with the same lifestyle strategies.
Impact on Heart Health
Both diseases target the cardiovascular system. Diabetes accelerates plaque formation through advanced glycation end‑products (AGEs), while hypertension adds mechanical stress that can rupture plaques. The combined effect raises the likelihood of coronary artery disease, heart failure, and stroke.
Patients with both conditions often develop left‑ventricular hypertrophy-a thickening of the heart’s main pumping chamber-earlier than those with a single diagnosis. Screening with an echocardiogram every 2‑3years is advised for adults over 40 who have both diagnoses.
Managing Both Conditions Together
Because the risk factors overlap, a unified management plan works best. Below is a step‑by‑step guide that addresses glucose, pressure, and overall heart health.
- Track daily numbers. Use a digital log or app to record fasting glucose, post‑meal glucose, and blood pressure each morning.
- Adopt a Mediterranean‑style diet. Aim for 45‑55% carbs from whole grains, legumes, and fruit; 15‑20% protein (lean fish, poultry, beans); 25‑35% healthy fats (olive oil, nuts). Limit added sugars to <10g per day and sodium to <1,500mg.
- Exercise consistently. Combine 150minutes of moderate aerobic activity (brisk walking, cycling) with two strength‑training sessions per week. Resistance work improves insulin sensitivity, while cardio lowers systolic pressure.
- Maintain a healthy weight. A 5‑10% weight loss can drop HbA1c by 0.5‑1% and systolic pressure by 5‑10mmHg.
- Manage stress. Mind‑body practices-meditation, yoga, or simply a 10‑minute deep‑breathing routine-cut cortisol spikes that raise both glucose and pressure.
- Limit alcohol and quit smoking. Alcohol >14 units/week and tobacco both raise blood pressure and impair glucose control.
- Review medications. Certain antihypertensives (ACE inhibitors, ARBs) protect kidney function in diabetics. Conversely, some diabetes drugs (SGLT2 inhibitors, GLP‑1 agonists) lower blood pressure as a side effect, offering a two‑in‑one benefit.
Always discuss any medication changes with your doctor; dosages might need tweaking when both conditions coexist.

When to Seek Professional Help
Even with diligent self‑care, some signals demand prompt medical attention:
- Consistently fasting glucose above 180mg/dL or a sudden rise in HbA1c (>2% increase).
- Systolic pressure persistently above 160mmHg or diastolic above 100mmHg despite lifestyle efforts.
- New chest pain, shortness of breath, or visual disturbances.
- Swelling in the ankles or unexplained weight gain-possible fluid retention from medication.
Early intervention can prevent irreversible organ damage.
Quick Checklist for Daily Success
- Log glucose & blood pressure each morning.
- Eat a balanced plate: half veg, quarter protein, quarter whole‑grain carbs.
- Move for at least 30minutes; mix cardio & strength.
- Stay under 1,500mg sodium; read labels.
- Hydrate (≈2L water) and limit sugary drinks.
- Practice a 5‑minute stress‑relief technique before bed.
Frequently Asked Questions
Can type 2 diabetes cause high blood pressure, or is it the other way around?
Both directions are possible. Insulin resistance promotes arterial stiffness, which raises pressure. At the same time, hypertension can impair blood flow to insulin‑sensitive tissues, worsening glucose control. The relationship is bidirectional.
Do I need separate doctors for each condition?
Not necessarily. A primary care physician experienced in chronic disease can coordinate care. However, if complications arise, a cardiologist or endocrinologist may become part of the team.
Are there foods that help lower both blood sugar and pressure?
Yes. Foods rich in magnesium and potassium-such as leafy greens, beans, nuts, and berries-support vascular health and improve insulin sensitivity. Oily fish (salmon, mackerel) provides omega‑3 fatty acids that dampen inflammation in both pathways.
How often should I get my blood pressure checked if I have diabetes?
At least once every clinic visit (usually every 3‑6months). If you’re on antihypertensive medication, home monitoring twice a week is advisable.
Can weight‑loss surgery help with both conditions?
Bariatric procedures often lead to rapid remission of type2 diabetes and significant reductions in blood pressure, especially when excess weight is the main driver. Eligibility criteria and long‑term follow‑up must be discussed with a specialist.
Xing yu Tao
October 13, 2025 AT 12:50Indeed, the interplay between insulin resistance and vascular tone exemplifies physiological interdependence.
Adam Stewart
October 16, 2025 AT 15:22When you look at the shared risk factors-obesity, excess sodium, and sedentary habits-it becomes clear that a single lifestyle overhaul can address both diabetes and hypertension simultaneously. Small, consistent changes often outweigh drastic, unsustainable measures.
Selena Justin
October 19, 2025 AT 17:53Maintaining regular monitoring of both glucose and blood pressure not only catches deviations early but also empowers you to adjust diet, activity, or medication promptly. Using a simple spreadsheet or a smartphone app can streamline this process without adding complexity to daily life.
Freddy Torres
October 22, 2025 AT 20:25Picture your arteries as highways; sugar spikes act like traffic jams while high pressure tries to speed‑up the flow, leading to inevitable crashes.
Andrew McKinnon
October 25, 2025 AT 22:57Wow, so you’re telling me that “insulin resistance” and “vascular stiffness” are basically BFFs? Groundbreaking insight-next you’ll announce that water is wet.
Dean Gill
October 29, 2025 AT 00:28First, understand that type 2 diabetes and hypertension share a common pathophysiological backbone: insulin resistance. When cells become less responsive to insulin, the pancreas compensates by secreting more, which in turn raises circulating insulin levels. Elevated insulin promotes sodium reabsorption in the kidneys, leading to fluid retention and higher blood pressure. Simultaneously, hyperglycemia induces oxidative stress, damaging the endothelial lining of blood vessels. This endothelial dysfunction reduces nitric oxide availability, a key vasodilator, further contributing to vasoconstriction. The resulting arterial stiffness not only raises systolic pressure but also impedes insulin delivery to peripheral tissues, creating a vicious feedback loop. Moreover, obesity-particularly visceral fat-releases adipokines that exacerbate both insulin resistance and inflammatory pathways. Chronic inflammation amplifies the atherogenic process, accelerating plaque formation and instability. As plaques grow, the heart must work harder, prompting left‑ventricular hypertrophy, a hallmark of long‑standing hypertension. The combined effect of metabolic and mechanical stress dramatically raises the risk of myocardial infarction and stroke. Lifestyle interventions, such as a Mediterranean‑style diet, target multiple mechanisms: they lower glycemic load, reduce sodium intake, and provide anti‑inflammatory nutrients like omega‑3 fatty acids. Regular aerobic exercise improves muscular glucose uptake, enhancing insulin sensitivity while also lowering resting heart rate and peripheral vascular resistance. Weight loss of even 5‑10 % can produce measurable reductions in both fasting glucose and systolic pressure. Pharmacologically, agents such as ACE inhibitors not only lower blood pressure but also improve renal insulin handling, offering dual benefits. Finally, consistent self‑monitoring creates a feedback loop that empowers patients to recognize patterns and intervene before complications arise.
Royberto Spencer
November 1, 2025 AT 03:00One could argue that our bodies are a series of contracts, each organ negotiating terms; when glucose breaches its agreement, blood pressure renegotiates, often to the detriment of both parties.
Annette van Dijk-Leek
November 4, 2025 AT 05:32Absolutely!!! The metaphorical contract is constantly being rewritten-sometimes in ink, sometimes in sweat!!!
Katherine M
November 7, 2025 AT 08:03⚖️ The bidirectional relationship between hyperglycemia and arterial pressure illustrates a delicate equilibrium; restoring balance requires both dietary discipline and vigilant monitoring. 🌿
Bernard Leach
November 10, 2025 AT 10:35Both conditions share core drivers such as excess adiposity excess sodium intake and sedentary behavior each factor amplifies the other's impact on cardiovascular health therefore a comprehensive approach that tackles weight reduction sodium moderation and regular physical activity is essential for risk mitigation
Shelby Larson
November 13, 2025 AT 13:07Look, you guys are basically re‑hashing the same bullet points. Everyone knows the basics-just quit the junk food already.
Mark Eaton
November 16, 2025 AT 15:38Hey folks, just a reminder: logging those numbers every morning can be a game‑changer. A quick glance at trends helps you spot spikes before they become emergencies.
Susan Cobb
November 19, 2025 AT 18:10While mainstream advice touts the Mediterranean diet, I maintain that a paleo‑centric regimen offers superior glycemic control and arterial health, albeit at the cost of culinary monotony.
Ivy Himnika
November 22, 2025 AT 20:42Interesting take-though the evidence still leans toward balanced plant‑forward meals for most patients 😊.
Nicole Tillman
November 25, 2025 AT 23:13Ultimately, individualized care plans, crafted with patient preferences and comorbidities in mind, deliver the best outcomes; one size does not fit all.
Sue Holten
November 29, 2025 AT 01:45Oh sure, because everyone loves eating kale all day while ignoring their cravings-totally realistic.
Tammie Foote
December 2, 2025 AT 04:17Reality check: sustainable changes beat extreme diets every time, no moral showdown needed.
Jason Ring
December 5, 2025 AT 06:48i think adding a short walk after dinner could help both sugar and pressure, just try it and see.
Neviah Abrahams
December 8, 2025 AT 09:20The silent killer lurks within, ready to strike when you least expect it; ignoring the signs is a gamble you cannot afford.
Uju Okonkwo
December 11, 2025 AT 11:50Remember, each step forward, no matter how small, builds momentum; celebrate progress and keep supporting one another on this journey.