Managing Indapamide-Induced Hypokalemia: A Practical Guide
15 Oct, 2025Potassium Management Calculator
Potassium Status Assessment
Helping you stay within the safe potassium range (3.5-5.0 mmol/L) while on indapamide therapy.
Indapamide‑induced hypokalemia is a medical condition characterized by reduced serum potassium levels caused by the thiazide‑like diuretic indapamide, which promotes potassium loss through the kidneys. If you or someone you care for is on indapamide for hypertension, knowing how to keep potassium in the safe zone can prevent muscle cramps, abnormal heart rhythms, and even hospitalization.
What Is Indapamide and Why Is It Prescribed?
Indapamide belongs to the thiazide‑like diuretics class. It works by relaxing the walls of blood vessels and increasing urine output, which lowers blood pressure. Doctors often choose it for patients who need a gentle yet effective antihypertensive that also offers some protection against calcium‑related kidney stones.
How Indapamide Lowers Potassium
The drug blocks sodium reabsorption in the distal convoluted tubule. When sodium stays in the urine, the kidney swaps it for potassium, pushing more potassium out of the body. Over weeks or months, this extra loss can drop serum potassium below the normal 3.5‑5.0mmol/L range, resulting in hypokalemia.
Spotting the Signs Early
Low potassium often sneaks up. Common clues include:
- Muscle weakness or twitches
- Fatigue that feels “out of proportion” to activity
- Irregular heartbeats (palpitations or skipped beats)
- Constipation or abdominal cramps
- Dry mouth or increased thirst
If you notice any of these while taking indapamide, don’t ignore them-check your potassium level.
How to Monitor Potassium Effectively
Regular lab work is the gold standard. Ask your clinician for a baseline potassium test, then repeat every 1‑3months during the first six months of therapy. If you’re on a higher dose (≥2.5mg daily) or have kidney disease, more frequent checks are wise.
Keep a simple log:
- Date of blood draw
- Result in mmol/L
- Any symptoms you felt that week
- Dietary changes you tried
This record helps your doctor see trends and decide whether to tweak the medication.

Boosting Potassium With Food
Dietary changes are the first line of defense. Aim for 2‑3 servings of potassium‑rich foods daily. Below is a quick comparison of common options.
| Source | Approx. K⁺ (mg per serving) | Convenience | Extra Benefits |
|---|---|---|---|
| Banana (1 medium) | 422 | Very easy | VitaminB6, fiber |
| Spinach cooked (½ cup) | d>420Medium | Iron, magnesium | |
| Sweet potato (1 cup, baked) | 540 | Easy | VitaminA, fiber |
| Orange juice (8oz) | 470 | Very easy | VitaminC |
| Potassium chloride tablet (20mmol) | ~780 | Very convenient | Rapid correction |
Fresh produce is best because it gives you fiber, vitamins, and antioxidants. If you can’t meet the target with food alone, a low‑dose supplement (typically 20‑40mmol potassium chloride) can fill the gap.
Choosing the Right Supplement
When a doctor recommends a supplement, they’ll consider kidney function and any heart‑rate‑affecting meds. Common choices include:
- Potassium chloride tablets - the standard, works quickly.
- Potassium citrate - also helps reduce urinary calcium, good if you have kidney stones.
- Slow‑release potassium - smoother absorption, fewer stomach upset.
Never double‑dose without medical approval; excess potassium can cause its own dangerous arrhythmias.
Medication Tweaks: When Diet Isn’t Enough
If potassium stays low despite food and a modest supplement, your clinician may adjust the drug regimen:
- Lower the indapamide dose (e.g., from 2.5mg to 1.5mg daily).
- Switch to a different antihypertensive that spares potassium, such as an ACE inhibitor or an ARB.
- Add a potassium‑sparing diuretic like spironolactone if blood pressure control still needs a second agent.
These changes should always be supervised, because abrupt dose cuts can raise blood pressure suddenly.
When to Call Your Healthcare Provider
Seek help right away if you notice any of the following:
- Palpitations, light‑headedness, or fainting
- Severe muscle cramps that don’t improve with rest
- Vomiting or diarrhea that could further deplete potassium
- Lab result showing potassium < 3.0mmol/L
In an emergency, call 000 (Australia) or go to the nearest emergency department.
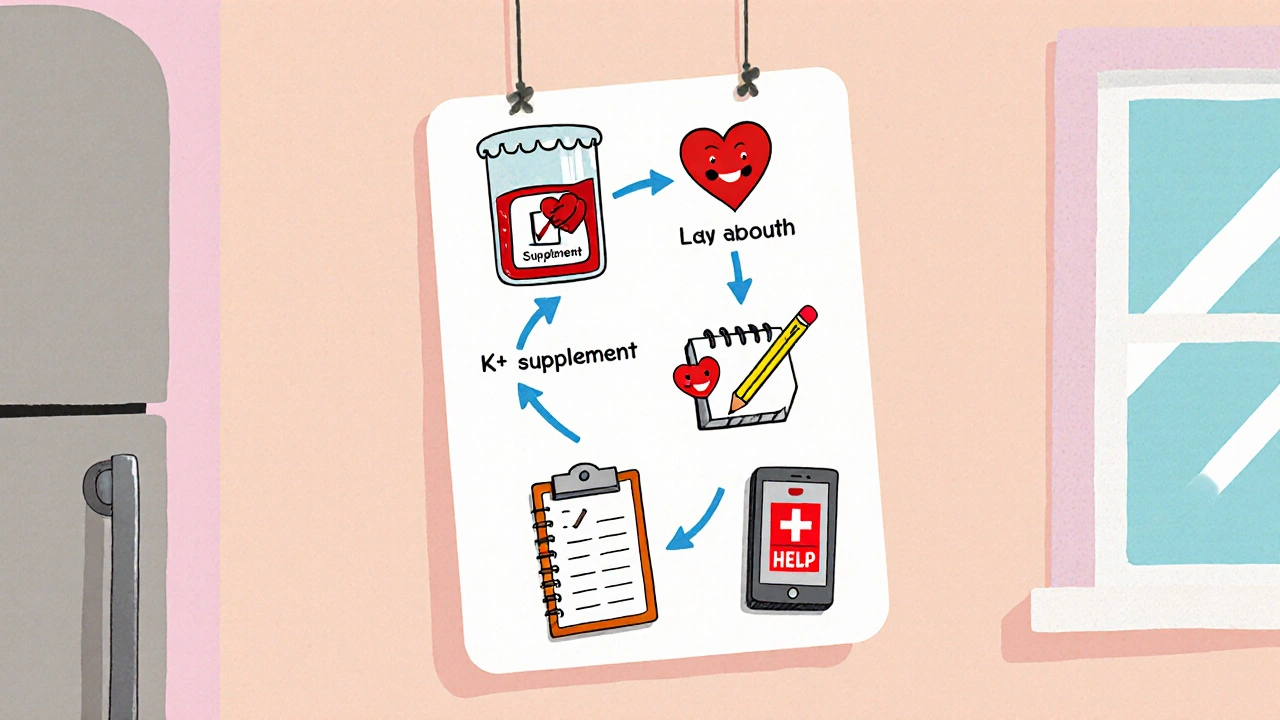
Quick Checklist for Managing Indapamide‑Induced Hypokalemia
- Get a baseline potassium level before starting indapamide.
- Schedule lab checks every 1‑3months for the first half‑year.
- Eat at least two potassium‑rich foods each day.
- Use a low‑dose supplement only if food falls short.
- Keep a symptom log and share it with your doctor.
- Ask about dose reduction or alternative meds if potassium stays low.
- Know the red‑flag symptoms that need urgent care.
Frequently Asked Questions
Can I stop indapamide on my own if I develop low potassium?
No. Stopping abruptly can cause a sudden rise in blood pressure and increase the risk of stroke. Always discuss dose changes with a clinician.
How fast can a potassium supplement raise my serum level?
A low‑dose tablet (20mmol) usually raises serum potassium by about 0.2‑0.3mmol/L within 4‑6hours, but the exact response varies with kidney function.
Are there any foods I should avoid while on indapamide?
High‑sodium foods (processed meats, canned soups, salty snacks) can counteract the blood‑pressure benefits and may worsen potassium loss. Aim for a low‑salt diet.
Is it safe to combine indapamide with a potassium‑sparing diuretic?
Yes, many clinicians pair a thiazide‑like diuretic with a low dose of spironolactone to balance potassium, but the combination requires regular labs to avoid hyper‑kalemia.
What level of potassium is considered dangerous?
Values below 3.0mmol/L are generally regarded as severe hypokalemia and increase the risk of life‑threatening arrhythmias.

M Black
October 15, 2025 AT 18:50Stay potassium‑rich, folks! 😊
Sidney Wachira
October 22, 2025 AT 17:30Oh wow, you think a simple banana can fix everything? Let me break it down for you: indapamide pulls potassium like a vacuum, and you need a strategic plan, not a snack. Think about balancing electrolytes with diet, labs, and maybe a low‑dose supplement. Trust me, I’ve read every guideline and lived it, so follow the checklist! 😎
Cinder Rothschild
October 29, 2025 AT 15:10When one first encounters the subtle, yet insidious, depletion of potassium caused by indapamide, the mind is immediately drawn to the cascade of physiological events that follow such an electrolyte imbalance. The sodium‑potassium exchange in the distal convoluted tubule becomes a relentless thief, stealing the vital mineral that sustains muscular and cardiac function. Over weeks of unnoticed loss, the body compensates with increasing fatigue and occasional muscle twitching, signals that are often dismissed as mere tiredness. Yet, each tremor is a herald of a deeper disturbance, a whisper that the serum potassium is slipping below safe thresholds. Regular monitoring therefore becomes not a suggestion but a moral imperative for anyone under this medication. Laboratory draws performed every one to three months capture the silent drift before it culminates in dangerous arrhythmias. The dietary regimen that follows should be both diverse and abundant, offering a colorful array of potassium‑rich foods from bananas to sweet potatoes, each contributing hundreds of milligrams per serving. It is essential to avoid high‑sodium processed foods, as sodium competes with potassium and amplifies loss. When diet alone proves insufficient, the judicious introduction of a low‑dose potassium chloride tablet can provide a rapid yet controlled rise in serum levels. Moreover, collaboration with a healthcare provider allows for dose adjustments of indapamide or the addition of a potassium‑sparing diuretic, creating a balanced therapeutic landscape. In the grand scheme, these measures weave together a safety net that protects against the dire consequences of hypokalemia. The importance of a symptom log cannot be overstated; it offers a narrative that clinicians can read to fine‑tune treatment. By embracing a proactive stance, patients transform themselves from passive recipients to active guardians of their electrolyte health. Each step, from lab work to dietary choice, builds upon the previous, forming a robust defense against the hidden threat of low potassium. Ultimately, the goal is not merely to survive the medication but to thrive while on it, maintaining optimal blood pressure control without compromising cardiac stability. Therefore, let us commit to vigilant monitoring, thoughtful nutrition, and open communication with our clinicians to master the management of indaprine‑induced hypokalemia.
Oscar Brown
November 5, 2025 AT 13:50It is a matter of both scientific rigor and philosophical prudence to recognize that the electrolyte milieu constitutes the very substrate upon which cellular homeostasis is predicated. In the dialectic of medicine, the thiazide‑like diuretic represents a vector of therapeutic benefit, yet its kinetic properties inexorably precipitate a potassium deficit. One must therefore contemplate the duality inherent in pharmacodynamics: amelioration of hypertensive pathology alongside the peril of hypokalemic sequelae. The physician, as a custodian of balanced biochemistry, must employ a regimented schedule of serum assays, thereby rendering the invisible, visible. Moreover, the lexicon of dietary intervention, enriched by potassium‑laden comestibles, should be enshrined within the therapeutic algorithm. It is not merely a recommendation but an ethical obligation to counsel patients on the ingestion of bananas, spinach, and sweet potatoes, each conferring a quantifiable millimole increase per serving. Should alimentary measures prove insufficient, the judicious addition of potassium chloride, calibrated to the patient’s renal function, becomes indispensable. Yet, this supplementation must be governed by the principle of iatrogenic caution, lest we transgress into hyper‑kalemic territory. The discourse extends further to encompass the potential synergy of a potassium‑sparing diuretic, an exemplar of pharmacological equilibrium. In sum, the management of indapamide‑induced hypokalemia is a microcosm of the broader medical endeavor: a harmonious balance of intervention, monitoring, and patient education, all underscored by an unwavering commitment to do no harm.
Tommy Mains
November 12, 2025 AT 12:30Here’s a quick rundown you can actually use: 1. Get your baseline K+ level before you start indapamide. 2. Schedule labs every 1‑3 months for the first six months. 3. Eat at least two servings of potassium‑rich foods a day – bananas, spinach, orange juice are all great. 4. If food isn’t enough, a low‑dose potassium chloride tablet (20‑40mmol) can fill the gap. 5. Keep a simple log of your blood draws, symptoms, and diet changes – it helps your doctor see trends. 6. Talk to your clinician about lowering the indapamide dose or adding a potassium‑sparing diuretic if labs stay low. 7. Watch for red‑flag symptoms like palpitations or severe cramps and call your provider right away. Following these steps should keep your potassium in the safe zone and your blood pressure under control.
Inma Sims
November 19, 2025 AT 11:10Ah, the noble art of potassium management – how delightfully straightforward when one merely adheres to a checklist, is it not? One might even suggest that if you can follow a recipe for a cake, you can certainly keep an eye on serum electrolytes, though the stakes, unlike a soufflé, involve your heart. Nevertheless, let us not overlook the occasional need for a splash of sarcasm when faced with overly‑simplified medical advice; after all, the human body rarely obeys a one‑size‑fits‑all formula.
Gavin Potenza
November 26, 2025 AT 09:50Think of it this way: the body is a tiny universe where potassium is the quiet philosopher keeping the stars in line. When indapamide nudges those electrons astray, it’s like a cosmic wobble – the solution is to bring balance back with the right food, the right meds, and a watchful eye on the labs. It’s a simple, elegant dance if you’re willing to listen to the rhythm of your own physiology.
Frank Pennetti
December 3, 2025 AT 08:30The whole thing is a textbook case of pharma‑driven iatrogenics – they slug you with indapamide to knock down blood pressure while silently siphoning potassium, then hand you a brochure about bananas like it’s a cure‑all. It’s a classic example of solutionist thinking wrapped in jargon‑heavy marketing, and the only real fix is a critical reassessment of dosing protocols, not just “add a supplement”.
Adam Baxter
December 10, 2025 AT 07:10Keep tracking labs and eat potassium foods daily 😊
Mariah Dietzler
December 17, 2025 AT 05:50i think it works but lol kinda hard to keep up
Nicola Strand
December 24, 2025 AT 04:30While the recommendations are sound, one must question whether universal application of such protocols disregards individual variability in renal handling of potassium.