MAOIs and Other Antidepressants: Combination Dangers and Safer Alternatives
4 Jan, 2026MAOI Drug Interaction Checker
Check Your Medication Combinations
This tool helps you identify safe and dangerous combinations with MAOIs. Always consult your doctor before making any medication changes.
Combining MAOIs with other antidepressants can be life-threatening-if you don’t know what you’re doing. Yet for some people with treatment-resistant depression, these older drugs are the only thing that works. The problem isn’t the MAOI itself. It’s the timing, the mix, and the lack of clear guidance. Many doctors avoid them entirely. But for those who’ve tried everything else, the right combination might be the difference between despair and relief.
Why MAOIs Are Still Used Today
Monoamine oxidase inhibitors (MAOIs) like phenelzine, tranylcypromine, and the selegiline patch aren’t first-line treatments. They’re not prescribed lightly. But they’re not outdated either. About 5-10% of psychiatrists still use them regularly, mostly for patients who haven’t responded to at least two other antidepressants. In fact, studies show that 40-60% of people with treatment-resistant depression improve on MAOIs-higher than most newer drugs.MAOIs work differently. Instead of just boosting serotonin like SSRIs, they stop the enzyme that breaks down serotonin, norepinephrine, and dopamine. That means more of all three mood-regulating chemicals stay active in the brain. This broad effect helps with symptoms like extreme fatigue, oversleeping, and emotional numbness-features often missed by other antidepressants.
The transdermal selegiline patch (Emsam) made things easier. At the lowest dose (6 mg/24 hours), you don’t need to avoid aged cheese or red wine. That’s why more people are using it now. But even with the patch, you still need to be careful about what else you take.
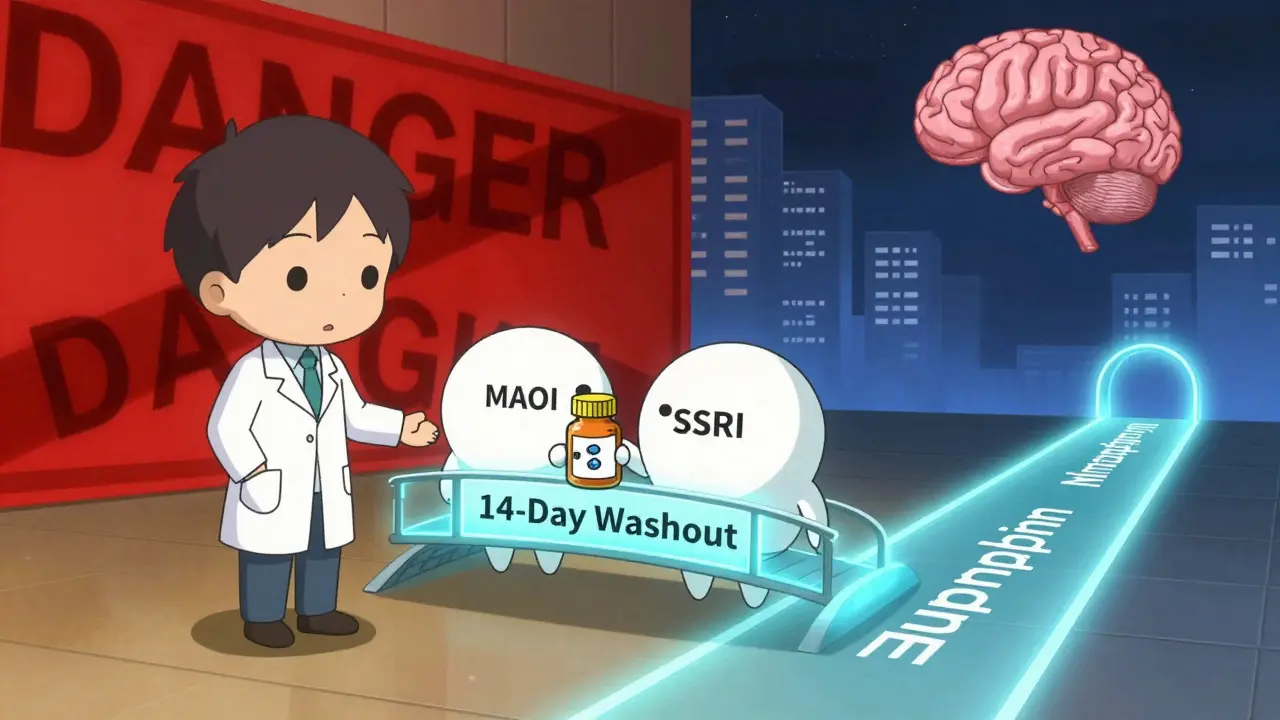
The Deadliest Mix: MAOIs and SSRIs/SNRIs
The most dangerous combination is MAOIs with SSRIs or SNRIs. This mix can trigger serotonin syndrome-a condition that can kill you in hours. Symptoms include high fever, muscle stiffness, rapid heartbeat, confusion, and seizures. In severe cases, your body overheats and shuts down.The FDA has a boxed warning on this. It’s not a suggestion. It’s a red alert. If you’ve been on fluoxetine (Prozac), you must wait five full weeks before starting an MAOI. Why? Fluoxetine sticks around longer than other SSRIs. Its active metabolite, norfluoxetine, can linger for up to two weeks after you stop. Other SSRIs like sertraline or escitalopram need at least 14 days off before an MAOI is safe.
And it’s not just one-way. If you’re on an MAOI and want to switch to an SSRI, you must wait 14 days after stopping the MAOI. Why? Your body needs time to rebuild the monoamine oxidase enzyme that the MAOI blocked. If you start an SSRI too soon, serotonin floods your system-and that’s when things go wrong.
A 1995 study in the Journal of Clinical Psychiatry looked at eight cases where people took fluoxetine and tranylcypromine together. Seven ended in death. That’s not a rare accident. It’s a predictable outcome.
What About Tricyclic Antidepressants (TCAs)?
The rules here are messier. Older guidelines said never combine MAOIs with TCAs. But recent research says: not so fast.Some TCAs, like clomipramine, are just as risky as SSRIs because they strongly block serotonin reuptake. Combining them with MAOIs is still a bad idea. But others-like nortriptyline-have weaker effects on serotonin. A 2022 review in PMC found that when used carefully, nortriptyline plus phenelzine worked well for treatment-resistant depression. In one study, 57% of patients responded with few side effects.
The key? Sequence matters. Never start the MAOI first. Start the TCA, let it stabilize, then add the MAOI slowly. If you reverse the order, you increase the chance of serotonin overload. This isn’t theoretical. Studies from the 1990s showed worse outcomes when MAOIs were introduced after TCAs.
Doctors who use this combo do it under close monitoring. Blood pressure, heart rate, and mental status are checked weekly. But it’s not for everyone. Only experienced prescribers should attempt it.
Safer Alternatives to Combine With MAOIs
You don’t have to stick to one drug. If MAOIs are your best option, you can still add other medications-just not the dangerous ones.Three antidepressants are generally safe to combine with MAOIs:
- Bupropion (Wellbutrin): It doesn’t affect serotonin. It works on dopamine and norepinephrine. No known risk of serotonin syndrome with MAOIs. Many clinicians use it to help with low energy or lack of motivation.
- Mirtazapine (Remeron): Works on different receptors and doesn’t block serotonin reuptake. Multiple case reports show it’s well-tolerated with MAOIs, even in severe depression.
- Trazodone: Used mostly for sleep, but also helps with mood. Low doses are safe with MAOIs. Just avoid high doses, which can increase serotonin slightly.
Even better? These aren’t just safe-they’re helpful. Bupropion can fix the sluggishness that SSRIs leave behind. Mirtazapine improves sleep and appetite, which are often broken in treatment-resistant depression. Trazodone helps with insomnia without the addiction risk of benzodiazepines.
Some doctors also add dopaminergic agents like pramipexole (used for Parkinson’s) to target anhedonia-the inability to feel pleasure. Case reports show improvement in motivation and emotional responsiveness when added to MAOIs. But this requires slow dosing and watching for impulse control issues like gambling or compulsive shopping.
What You Can Also Take Safely
You don’t need to suffer side effects alone. Many common medications are safe with MAOIs:- Benzodiazepines (like lorazepam or clonazepam): Great for anxiety or panic attacks that come with depression.
- Non-benzodiazepine sleep aids (like zolpidem or eszopiclone): Help with insomnia without serotonin interaction.
- Antihistamines (like diphenhydramine): Safe for allergies or sleep, but avoid decongestants like pseudoephedrine-they can spike blood pressure.
Just remember: if a medication affects serotonin, dopamine, or norepinephrine, check before combining. Even OTC cold medicines can be risky.
Dietary Restrictions Still Matter
Even if you’re on the selegiline patch, you can’t ignore food. At higher patch doses (above 6 mg/24hr), you need to avoid high-tyramine foods. That means:- Aged cheeses (Parmesan, blue cheese, cheddar)
- Tap beer and draft wine
- Fermented meats (salami, pepperoni)
- Soy sauce, miso, and fermented tofu
- Overripe bananas and avocados
Why? Tyramine builds up in these foods. Normally, your body breaks it down with monoamine oxidase. But if that enzyme is blocked by an MAOI, tyramine floods your system. That causes a sudden, dangerous spike in blood pressure-sometimes over 200 mmHg. It can lead to stroke or heart attack.
And you still need to avoid these foods for two weeks after stopping the MAOI. Your enzyme levels haven’t fully recovered yet.

Stopping MAOIs Isn’t Simple
You can’t just quit. Abruptly stopping an MAOI causes withdrawal symptoms that feel like the flu-but worse:- Restlessness (62% of people)
- Upset stomach (48%)
- Tingling or burning skin (37%)
- Flu-like symptoms (55%)
- Insomnia (71%)
- Headaches (68%)
That’s not just discomfort. It’s a real withdrawal syndrome. Always taper slowly-over two to four weeks. Your doctor should guide this. Don’t cut pills in half and hope for the best.
Who Should Avoid MAOIs Altogether?
Not everyone is a candidate. Avoid MAOIs if you:- Have uncontrolled high blood pressure
- Have liver disease
- Are pregnant or breastfeeding
- Have a history of stroke or heart attack
- Are under 18 (limited safety data)
Also, if you’ve ever had serotonin syndrome before, MAOIs are off the table. The risk of recurrence is too high.
The Bottom Line
MAOIs aren’t the answer for everyone. But for the 15-20% of people with depression that won’t budge with other drugs, they’re often the only option left. The danger isn’t the drug-it’s the ignorance around it.Use them safely: know the washout periods, avoid the deadly combos, stick to the safe alternatives, and never skip the diet rules. Work with a psychiatrist who’s done this before. If your doctor says, "I don’t prescribe MAOIs," ask why. Maybe they’re scared. Or maybe they just haven’t learned the right way to use them.
For some, MAOIs aren’t a last resort. They’re the best shot at getting back to life.
Can I take SSRIs after stopping an MAOI?
Yes, but you must wait at least 14 days after stopping the MAOI. If you were on fluoxetine (Prozac) before the MAOI, you need to wait five weeks before restarting it. This is because fluoxetine and its metabolite stay in your system much longer than other SSRIs. Starting too soon can trigger serotonin syndrome, which can be fatal.
Is it safe to combine MAOIs with bupropion?
Yes, bupropion is one of the safest antidepressants to combine with MAOIs. It doesn’t affect serotonin reuptake-it works on dopamine and norepinephrine. Many clinicians use this combo for patients with low energy, lack of motivation, or anhedonia. No cases of serotonin syndrome have been reliably linked to this combination.
Why are MAOIs not prescribed more often?
Most doctors avoid MAOIs because of the complex drug interactions, dietary restrictions, and fear of side effects. Only 32% of psychiatry residents feel confident managing them. Many aren’t trained in the safe sequencing of medications or how to monitor patients. As a result, even though MAOIs are highly effective for treatment-resistant depression, they’re underused.
Can I drink alcohol while on an MAOI?
It’s best to avoid alcohol entirely. Alcohol can interact with MAOIs and cause dangerous spikes in blood pressure. Some types, like red wine and tap beer, also contain tyramine, which can trigger a hypertensive crisis. Even small amounts can be risky, especially with older MAOIs like phenelzine. The selegiline patch is safer at low doses, but alcohol still increases drowsiness and dizziness.
What’s the difference between the MAOI patch and pills?
The selegiline patch (Emsam) delivers the drug through the skin, which reduces how much of it enters your bloodstream all at once. At the lowest dose (6 mg/24hr), you don’t need to follow strict dietary restrictions. Higher doses (9 mg and 12 mg) still require avoiding tyramine-rich foods. Pills like phenelzine and tranylcypromine affect your entire system, so dietary rules apply no matter the dose.
How long does it take for MAOIs to work?
Most people start noticing improvement in 2-4 weeks, but full effects can take 6-8 weeks. Unlike SSRIs, which often help with anxiety first, MAOIs tend to improve energy, motivation, and mood together. That’s why they’re preferred for atypical depression-where fatigue and emotional numbness dominate.
Can I use MAOIs if I’ve tried multiple antidepressants and still feel hopeless?
Yes. MAOIs are specifically used for treatment-resistant depression-when two or more other antidepressants failed. Studies show 40-60% of these patients respond to MAOIs. If you’ve tried SSRIs, SNRIs, and even TCAs without relief, MAOIs may be your best option. But you need to work with a psychiatrist experienced in their use. Don’t give up-this isn’t the end of the road.

Katelyn Slack
January 5, 2026 AT 13:26ive been on selegiline patch for 8 months and honestly its been a game changer. no more cheese anxiety, just a quiet lift. i still avoid red wine tho, better safe than sorry. also bupropion helped with my morning fog. thanks for this post, it’s the first time i felt understood.
Stuart Shield
January 7, 2026 AT 06:57man, this is the kind of post that makes you feel like you’re not alone in the dark. i’ve been on phenelzine for three years, and yeah, the dietary rules are a pain-but when you finally stop feeling like a ghost in your own body, you learn to live with the rules. i keep a little cheat sheet taped to my fridge. ‘no blue cheese, no tap beer, no soy sauce after 6pm.’ sounds silly, but it’s my lifeline. also, trazodone at night? pure gold. sleep without nightmares? miracle.
Tiffany Adjei - Opong
January 8, 2026 AT 11:23ok but why are we still using 1950s drugs when we have ketamine and psilocybin trials going on? MAOIs are basically the medical equivalent of using a flip phone in 2024. sure, they work-but it’s like using a hammer to install a wifi router. also, who still eats aged cheese? that’s just a lifestyle choice, not a medical necessity. 🤷♀️
Tom Swinton
January 9, 2026 AT 06:01I just want to say-this post is a godsend. I’ve been on MAOIs for 5 years, and I’ve had doctors tell me I’m ‘too complicated’ or ‘not a good candidate.’ But here’s the truth: I was suicidal. I couldn’t get out of bed. I cried every morning. Then I tried phenelzine. Slowly, I started to feel like ME again. Not perfect. Not fixed. But present. And yes, I avoid tyramine like it’s a curse. But I’d rather live with a boring diet than die from a foggy mind. To anyone reading this who’s been told ‘there’s nothing left’-there is. MAOIs aren’t the end. They’re the bridge. And you deserve to cross it.
Saylor Frye
January 9, 2026 AT 06:33MAOIs? Really? That’s so… 1980s. I mean, if you’re not on esketamine or TMS, are you even trying? Also, why are you still talking about cheese? It’s 2024. We have lab-grown soy sauce now. 🤓
Kiran Plaha
January 10, 2026 AT 22:29my uncle took phenelzine back in the 90s. he said he felt alive for the first time since he was 18. he still avoids soy sauce. he says it’s worth it. i never thought i’d say this but… maybe we should listen to the old guys more.
Kelly Beck
January 11, 2026 AT 14:07YOU ARE NOT ALONE 💪💖 I’ve been where you are. I thought I’d never feel joy again. Then I found my psychiatrist who actually knew how to use MAOIs. Bupropion + patch = my new best friends. I cry less. I laugh more. I even went hiking last weekend. 🌿✨ You’ve got this. Keep going. Your light is still on. ❤️
Isaac Jules
January 13, 2026 AT 07:56Wow. Another person who thinks MAOIs are magic. Let me guess-you also think vitamin D cures cancer? This post is dangerous. People die from serotonin syndrome. You’re glorifying a drug that’s basically a chemical grenade. And now you want people to combine it with trazodone? Are you serious? This isn’t self-help-it’s a suicide checklist. 🚨
Amy Le
January 14, 2026 AT 19:49MAOIs? In America? That’s just cultural backwardness. In India, they use ayurvedic herbs and meditation. In Germany, they use light therapy. Why are we still playing Russian roulette with brain chemistry? This is why our healthcare system is broken. 🇺🇸💀
Pavan Vora
January 16, 2026 AT 14:33in india, we have a saying: 'the old medicine remembers what the new medicine forgets.' my grandmother used to say that about turmeric and depression. i didn't believe her until i tried maois. now i take the patch and eat rice with lentils. no cheese, no wine, but i sleep. and that's enough.
Indra Triawan
January 17, 2026 AT 04:41the real tragedy isn’t the MAOIs-it’s that we treat depression like a math problem. fix the serotonin, fix the dopamine, fix the life. but what if the problem isn’t the brain? what if it’s the world? why are we so quick to chemically silence pain instead of changing the conditions that cause it? just saying.
Ashley S
January 19, 2026 AT 01:20if you’re on MAOIs, you’re basically a medical experiment. why not just take a vacation? or get a dog? or go to therapy? why do you need chemicals to feel human? this is just laziness disguised as science.
Jeane Hendrix
January 19, 2026 AT 14:46the bupropion + MAOI combo is legit. i’ve been on it for 2 years. no serotonin syndrome. no dietary panic. just steady energy. also, the patch is way better than pills-less GI distress. i wish more docs knew this. most still think it’s a death sentence. it’s not. it’s a second chance.
Harshit Kansal
January 19, 2026 AT 23:30my cousin took phenelzine and stopped because he missed his mom’s birthday dinner. she made homemade cheese. he ate it. ended up in the ER. now he says he’d rather be sad than scared. i get it. but man… it’s a heavy tradeoff.
Melanie Clark
January 20, 2026 AT 05:03you know who really benefits from MAOIs? The pharmaceutical companies. They make more money off the combo drugs and the endless monitoring. And the diet restrictions? That’s just to keep you dependent. The real cure is systemic change. Trauma. Poverty. Loneliness. Not some enzyme blocker. This is a distraction. They want you to think you’re fixed when the world is still broken. Wake up.