Secondary Hypogonadism and Anemia: How Low Testosterone Affects Red Blood Cells
4 Oct, 2025Secondary Hypogonadism & Anemia Risk Calculator
Please answer the following questions about your symptoms and health status to assess your risk of developing anemia due to secondary hypogonadism:
Your Risk Assessment
Ever wondered why men with low testosterone sometimes feel unusually tired or short‑of‑breath? The missing link is often anemia, a condition where the blood can’t carry enough oxygen. This article unpacks the relationship between secondary hypogonadism and anemia, walks you through the science, symptoms, diagnosis, and practical steps to get back on track.
What Exactly Is Secondary Hypogonadism?
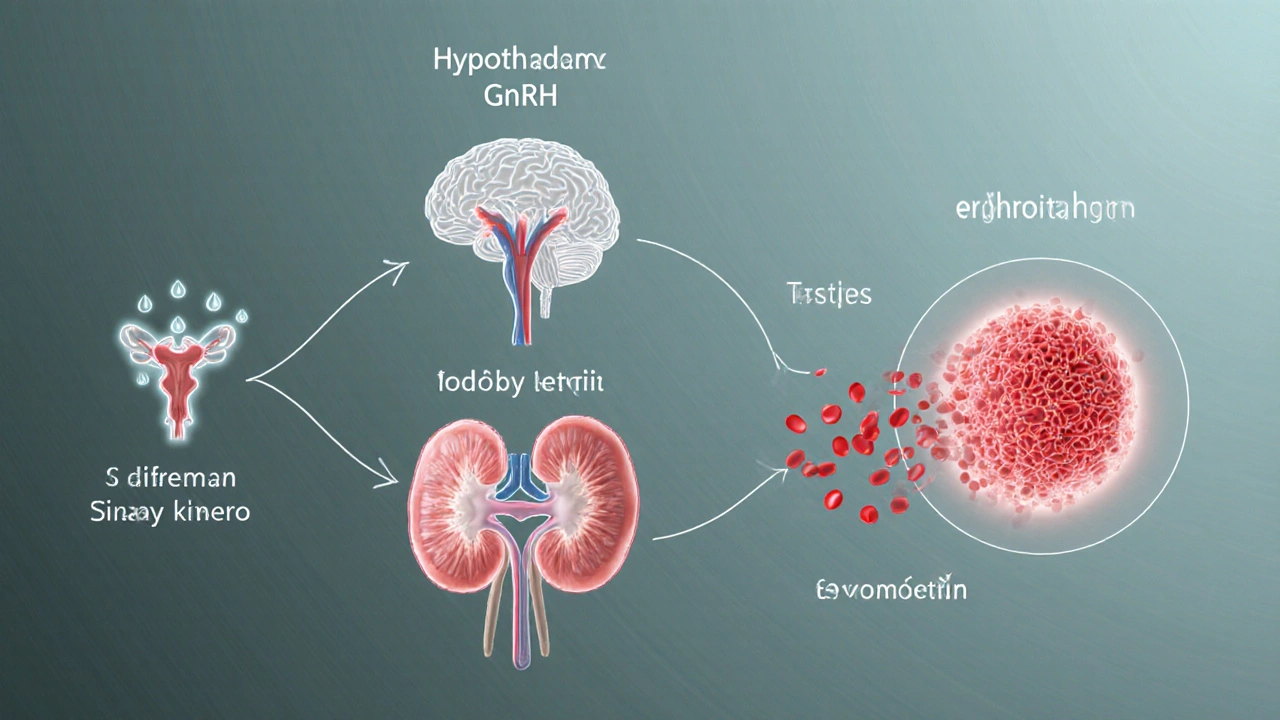
Secondary hypogonadism is a hormonal disorder in which the testes produce insufficient testosterone because the brain’s pituitary or hypothalamus fails to signal properly. Unlike primary hypogonadism, where the testicles themselves are damaged, secondary cases stem from problems higher up the chain-think pituitary tumors, chronic stress, or certain medications.
Understanding Anemia in Simple Terms
Anemia refers to a reduction in the number of healthy red blood cells or the amount of hemoglobin they contain, leading to reduced oxygen delivery to tissues. Common forms include iron‑deficiency anemia, anemia of chronic disease, and, less well known, anemia caused by hormonal imbalances.
Why Low Testosterone Can Lead to Low Red Blood Cells
The connection isn’t magic-it’s biology. Testosterone stimulates the kidney’s production of erythropoietin a hormone that tells the bone marrow to make more red blood cells. When testosterone drops, erythropoietin levels fall, and the bone marrow slows its output. Over time, this can tip a healthy blood count into the anemia range.
Key Players in the Hormone‑Blood Axis
- Testosterone the primary male sex hormone that regulates muscle mass, libido, and red blood cell production.
- Pituitary gland the master endocrine organ that releases luteinizing hormone (LH) to stimulate testosterone synthesis.
- Hypothalamus the brain region that secretes gonadotropin‑releasing hormone (GnRH) to cue the pituitary.
- Iron a mineral essential for hemoglobin formation; deficiency can worsen anemia caused by low testosterone.
- Chronic kidney disease a condition that reduces erythropoietin output, compounding the effect of testosterone deficiency.
- Inflammatory cytokines molecules like IL‑6 that suppress both testosterone production and iron utilization.
Common Scenarios Where the Two Meet
| Cause | Effect on Testosterone | Effect on Red Blood Cells |
|---|---|---|
| Pituitary tumor | Decreased LH → Lower testosterone | Reduced erythropoietin stimulation → Anemia |
| Long‑term corticosteroid therapy | Suppresses GnRH/LH axis | Bone‑marrow suppression + iron loss → Anemia |
| Chronic kidney disease | Impaired conversion of testosterone to its active form | Low erythropoietin output → Anemia |
| Severe obesity | Elevated aromatase converts testosterone to estrogen | Inflammation reduces iron availability → Anemia |
| HIV or hepatitis C infection | Direct viral impact on hypothalamic-pituitary axis | Chronic inflammation + medication side‑effects → Anemia |
Symptoms You Might Notice
Both conditions share fatigue, but each adds its own flavor. Look out for:
- Persistent tiredness that doesn’t improve with rest (anemia)
- Reduced libido, erectile dysfunction, or loss of facial hair (low testosterone)
- Shortness of breath during light activity (anemia)
- Muscle weakness, especially in the thighs and arms (both)
- Mood swings or mild depression (hormonal imbalance)
- Cold intolerance or pale skin (anemia)
How Doctors Diagnose the Overlap
Diagnosis is a step‑by‑step process that combines blood work, imaging, and a focused history.
- Hormone panel: Measure total and free testosterone both total and bioavailable levels to confirm hypogonadism.
- Complete blood count (CBC): Look for low hemoglobin, hematocrit, and red blood cell count - hallmarks of anemia.
- Erythropoietin level: Low values point toward a hormonal cause rather than iron deficiency.
- Iron studies: Serum ferritin, transferrin saturation, and total iron‑binding capacity differentiate iron‑deficiency anemia from anemia of chronic disease.
- Imaging: MRI of the pituitary or CT scan if a tumor is suspected.
- Additional labs: Thyroid function, cortisol, and inflammatory markers (CRP, IL‑6) to rule out other endocrine or inflammatory contributors.
Treatment Pathways - What Works When Both Conditions Co‑Exist
Therapy usually tackles two fronts: raising testosterone and correcting the anemia.
1. Testosterone Replacement Therapy (TRT)
- Forms: injections (e.g., testosterone cypionate), transdermal gels, or buccal tablets.
- Goal: bring serum testosterone into the mid‑normal male range (400‑600ng/dL).
- Effect on anemia: many studies show a 10‑20% rise in hemoglobin after 3‑6months of adequate TRT.
2. Addressing the Anemia Directly
- If iron‑deficiency is present, oral ferrous sulfate 325mgTID for 3months, followed by maintenance.
- For anemia of chronic disease, erythropoiesis‑stimulating agents (ESAs) like darbepoetin may be used, but only after TRT has been optimized.
- Vitamin B12 or folate supplementation when deficiencies are identified.
3. Lifestyle Tweaks That Boost Both Hormones and Blood
- Weight loss: dropping 5‑10% body weight can raise testosterone by up to 15%.
- Resistance training: 3‑4 sessions per week stimulate natural testosterone spikes and improve bone‑marrow health.
- Sleep hygiene: aim for 7‑9hours; poor sleep lowers LH and raises cortisol, worsening both conditions.
- Limit alcohol and avoid nicotine - both blunt testosterone and impair iron absorption.
Potential Pitfalls and How to Avoid Them
Even with a solid plan, a few common mistakes can derail progress.
- Skipping follow‑up labs: Hormone levels can fluctuate; check testosterone and CBC every 3‑6months.
- Over‑relying on oral iron: Gastrointestinal side‑effects lead to poor adherence. Consider liquid iron or IV iron if oral fails.
- Ignoring underlying disease: If a pituitary tumor is the root cause, surgery or radiotherapy might be needed before TRT will work.
- Using exogenous testosterone without monitoring: Excess can raise hematocrit >52%, increasing clot risk. Therapeutic phlebotomy may be required.
When to See a Specialist
If you experience any of the following, book an appointment with an endocrinologist or a hematologist:
- Persistent fatigue despite iron supplements.
- Sudden drop in libido or erectile function.
- Shortness of breath at rest or with minimal activity.
- Headaches, vision changes, or unexplained weight loss - red flags for pituitary lesions.
- Hematocrit consistently above 52% while on TRT.
Bottom‑Line Checklist for Managing Secondary Hypogonadism‑Related Anemia
- Get baseline labs: total & free testosterone, CBC, ferritin, erythropoietin.
- Identify the root cause (pituitary, medication, chronic disease).
- Start testosterone replacement if confirmed low.
- Treat iron deficiency or give ESA only after testosterone is stable.
- Re‑check labs in 3 months, adjust dose, and monitor hematocrit.
- Incorporate resistance training, adequate sleep, and weight control.
- Seek specialist care if symptoms persist or labs don’t improve.

Frequently Asked Questions
Can low testosterone cause anemia on its own?
Yes. Testosterone directly stimulates erythropoietin production, so when levels fall, red‑blood‑cell output can dip enough to meet anemia criteria, especially if other risk factors like poor nutrition are present.
Is testosterone therapy safe for men with anemia?
Generally yes, but doctors must monitor hematocrit. If it rises above 52%, a therapeutic phlebotomy or dose reduction may be needed to avoid clotting risks.
How long does it take for hemoglobin to improve after starting TRT?
Most men see a measurable rise within 8‑12 weeks, with the greatest change by six months. The exact timing varies based on baseline testosterone, age, and whether iron stores are adequate.
Do I need iron supplements if my doctor starts me on TRT?
Only if iron studies show deficiency. TRT can raise hemoglobin, but without enough iron the bone marrow can’t produce new cells efficiently, so checking ferritin first is essential.
Can lifestyle changes replace medication?
In mild cases, losing weight, exercising, and improving sleep can lift testosterone enough to normalize blood counts. However, moderate to severe hypogonadism usually still requires medical therapy.

Sangeeta Birdi
October 4, 2025 AT 02:49Feeling low? Take care of yourself and get those labs checked. 💙
Chelsea Caterer
October 11, 2025 AT 01:29This is a solid breakdown its helpful.
Lauren Carlton
October 18, 2025 AT 00:09The article has a few grammatical hiccups; for instance, "secondary hypogonadism" should be hyphenated consistently and commas are missing before many list items. Also, the term "low T" is informal; stick with "low testosterone" for clarity.
Katelyn Johnson
October 21, 2025 AT 11:29I see your point but maybe we can add that testosterone also impacts mood and energy levels, which ties back to anemia symptoms.
Elaine Curry
October 24, 2025 AT 22:49Honestly the article never mentioned diet, that's a huge oversight.
Patrick Fortunato
October 31, 2025 AT 20:29As an Irish lad I've seen men struggling with low T, proper testing is key.
Manisha Deb Roy
November 7, 2025 AT 19:09Testosterone deficiency does more than lower libido; it also hampers red blood cell production. The kidney’s erythropoietin output drops when testosterone levels fall, leading to a subtle anemia. When evaluating a patient, start with a full hormone panel including total and free testosterone. Pair that with a complete blood count to spot any drops in hemoglobin or hematocrit. Iron studies should follow if the CBC suggests anemia, checking ferritin, transferrin saturation, and TIBC. If iron stores are adequate, consider measuring serum erythropoietin to differentiate causes. Imaging, such as a pituitary MRI, is warranted when secondary hypogonadism is suspected. Lifestyle interventions like resistance training can naturally boost testosterone by up to 15 percent. Weight loss of just five to ten percent body weight often improves both hormone levels and inflammatory markers. Adequate sleep-seven to nine hours-prevents cortisol spikes that suppress luteinizing hormone. Once testosterone replacement therapy is initiated, monitor hematocrit every three months. A rise above 52 percent may require dose adjustment or therapeutic phlebotomy to mitigate clot risk. Iron supplementation should only be added if ferritin is low; otherwise, oral iron can cause gastrointestinal upset. For anemia of chronic disease, erythropoiesis‑stimulating agents are an option but only after testosterone is stable. Patient education on recognizing symptoms of excess red cells-headaches, visual changes-is essential. Finally, maintain open communication with both endocrinology and hematology specialists to coordinate care effectively.
Helen Crowe
November 11, 2025 AT 06:29From a hematology perspective, erythropoietin dynamics are crucial; low testosterone reduces renal EPO secretion, which then limits marrow erythropoiesis. Adding iron repletion without addressing the hormonal deficit may only give a partial response. Combining TRT with iron therapy, when indicated, yields synergistic improvements in hemoglobin. Monitoring reticulocyte counts can help gauge marrow response after therapy adjustments. Keep an eye on hematocrit to avoid polycythemia when testosterone levels rise.
Anthony Aspeitia-Orozco
November 18, 2025 AT 05:09Great overview, remember to set realistic goals for lab improvements and track symptoms over time.
Adam Dicker
November 21, 2025 AT 16:29Listen up! The iron deficiency angle is often ignored! You need to check ferritin before you start any testosterone shots! Otherwise you’ll just mask the real problem! Get those labs done, then tailor the therapy!
Molly Beardall
November 28, 2025 AT 15:09The article's structure is flawless, yet some sections could benefit from clearer headings.
Brian Pellot
December 2, 2025 AT 02:29I agree, a clear heading helps readers navigate complex topics.
Patrick McCarthy
December 9, 2025 AT 01:09What about the role of inflammation in suppressing both hormones?
Geraldine Grunberg
December 12, 2025 AT 12:29Excellent question! Indeed, inflammatory cytokines-particularly IL‑6-play a pivotal role; they can reduce testosterone production and impair iron metabolism.
Elijah Mbachu
December 19, 2025 AT 11:09Take it one step at a time; small changes add up.